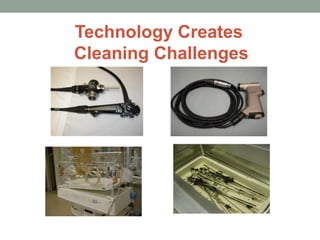
This document discusses guidelines for cleaning and decontamination in a healthcare setting. It covers factors that impact the cleaning process like facility design, environmental controls, and staff safety. It also describes selection and use of cleaning agents like water, detergents, and enzymes. Manual and mechanical cleaning methods are explained including cleaning of different instrument types. Procedures for managing infectious waste and staff training are also outlined.