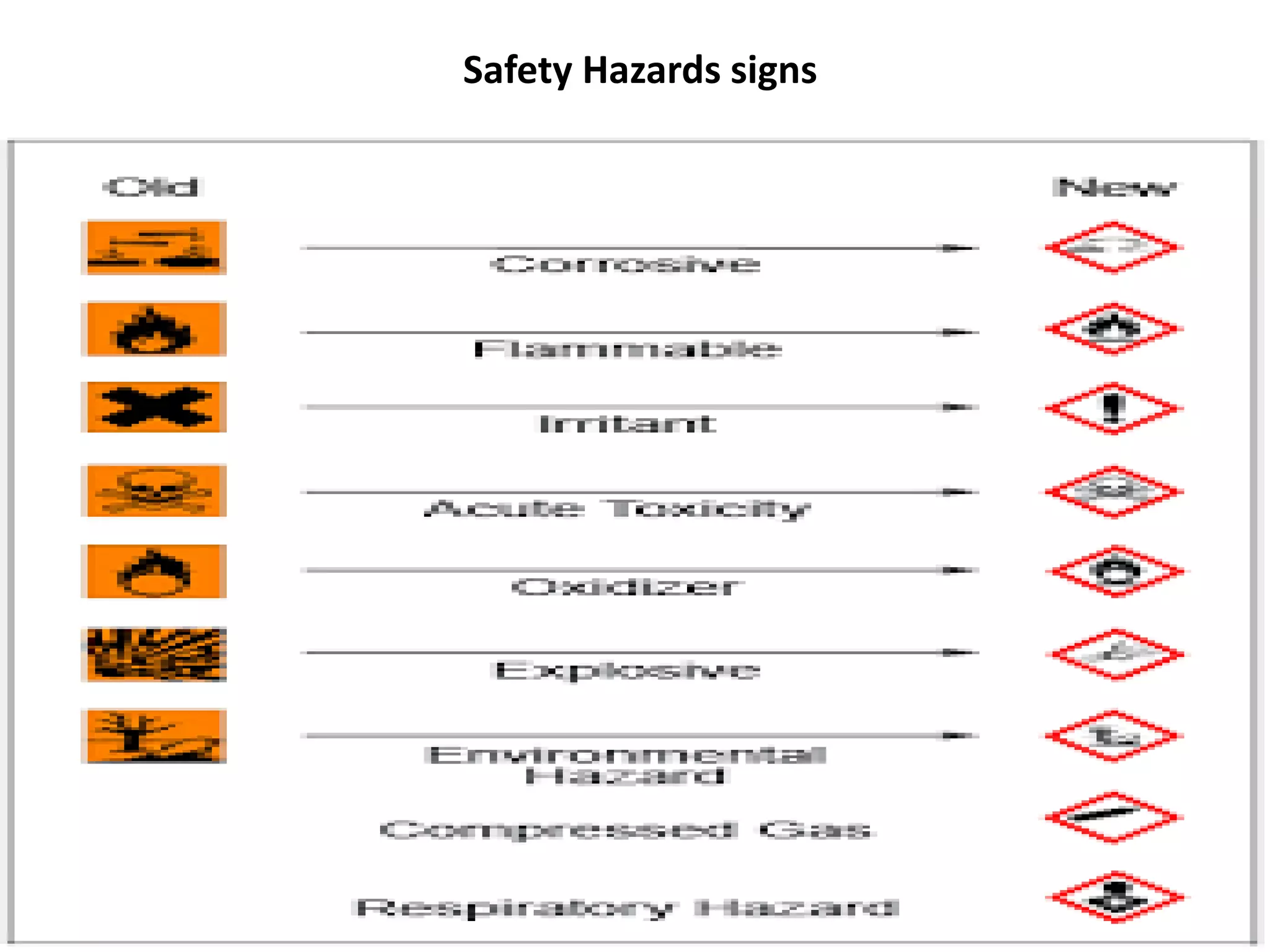
The document outlines various hazards associated with running a research laboratory, categorizing them into chemical, biological, and physical hazards, each posing significant risks to worker health and safety. It emphasizes the importance of recognizing these hazards, implementing safety protocols, and utilizing appropriate sterilization methods to minimize contamination and ensure safety. Additionally, general laboratory safety practices are emphasized to prevent incidents and ensure a safe working environment.