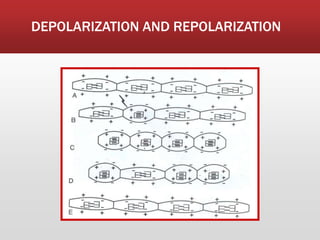
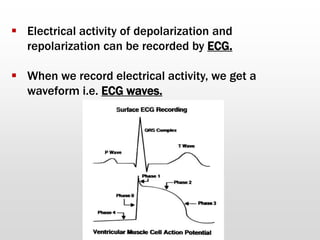
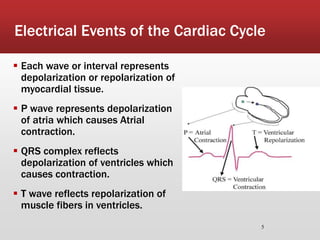
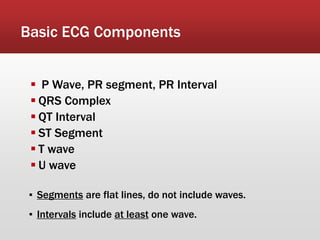
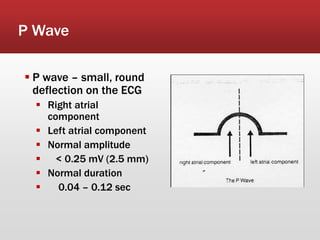
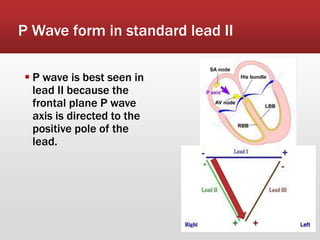
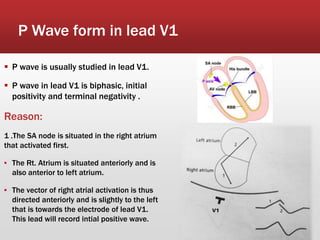
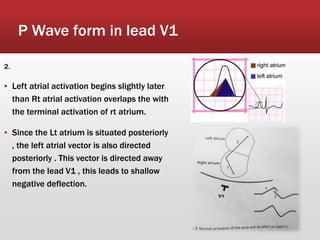
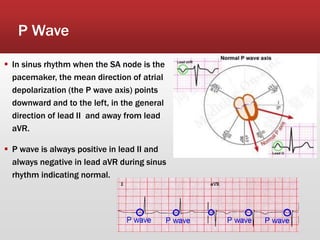
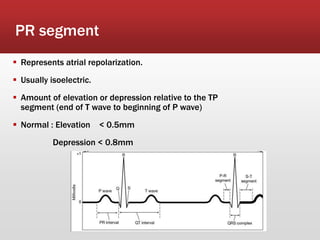
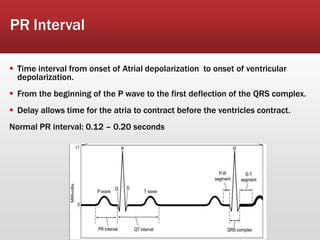
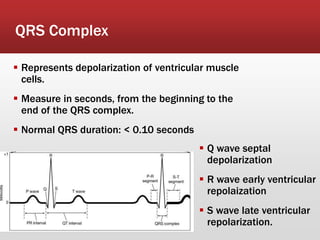
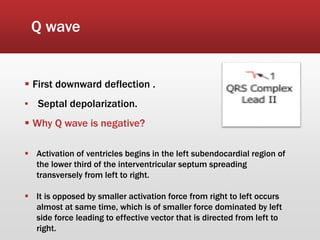
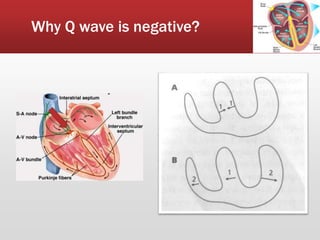
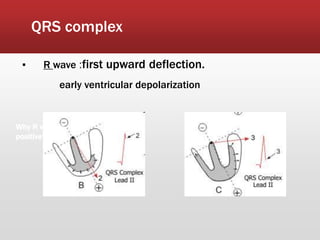
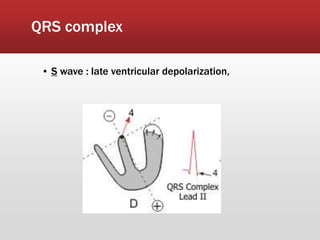
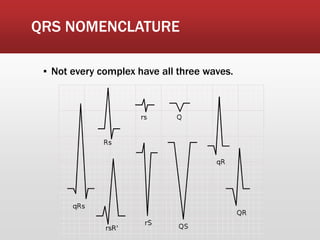
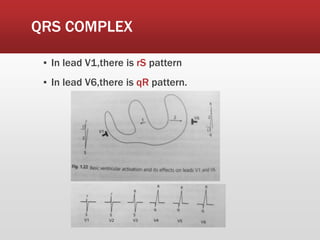
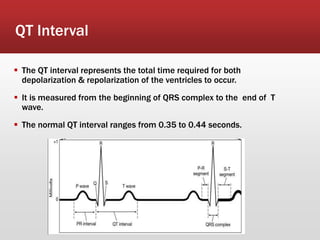
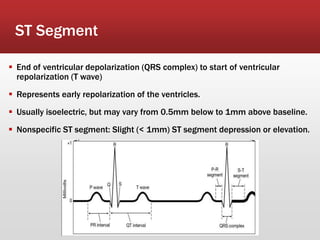
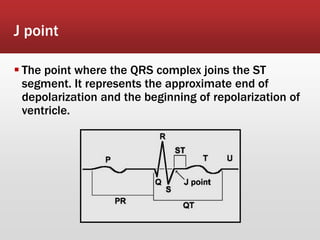
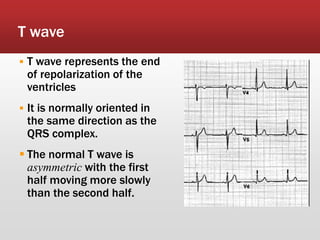
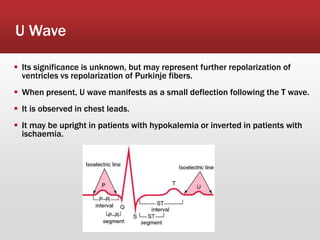
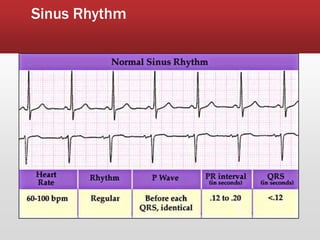
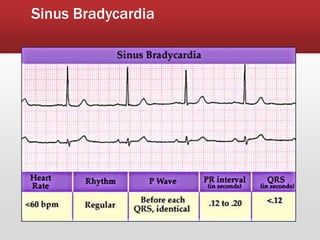
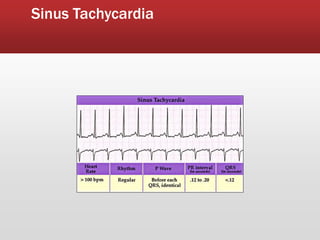
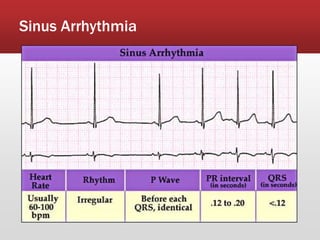
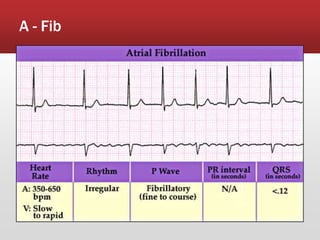
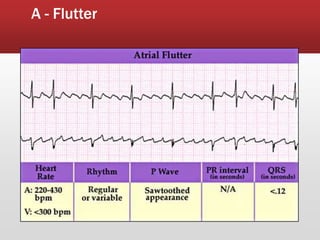
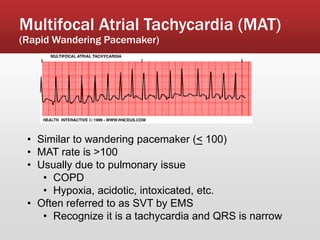
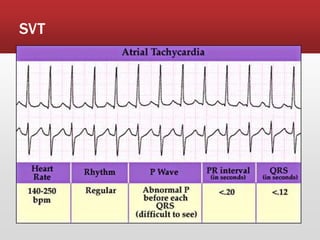
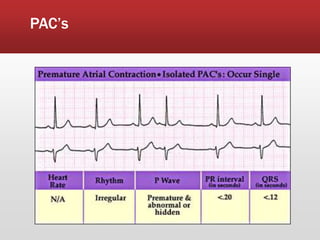
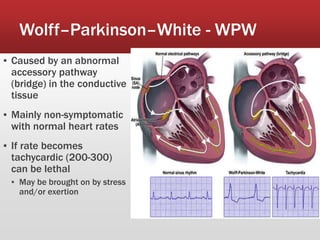
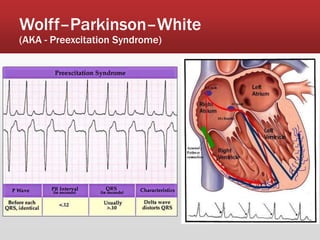
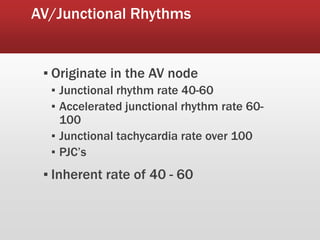
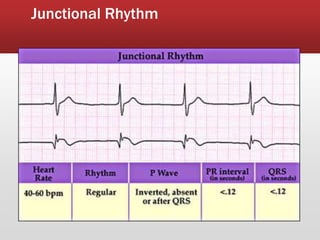
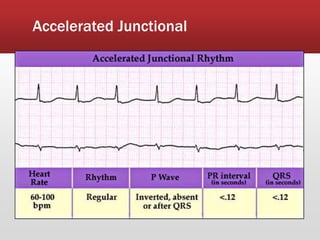
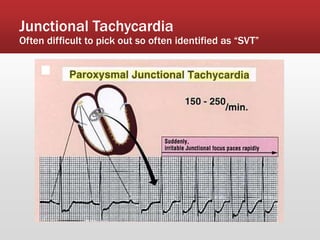
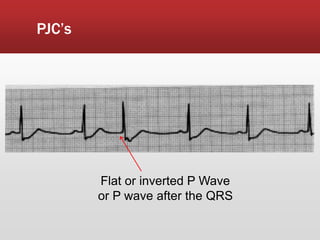
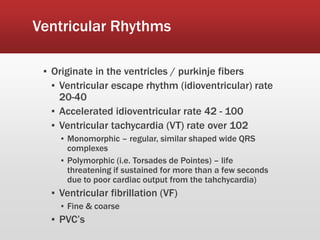
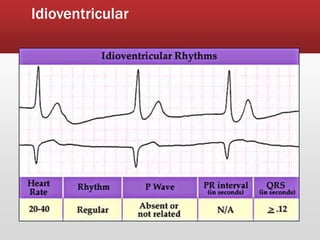
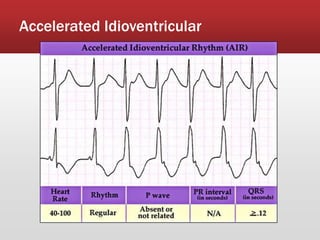
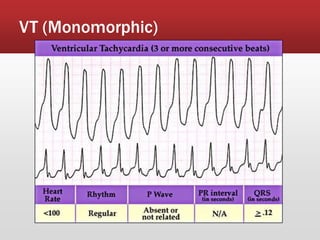
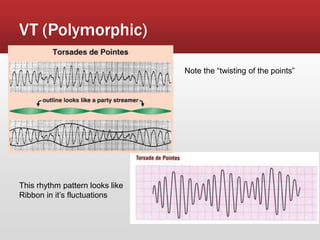
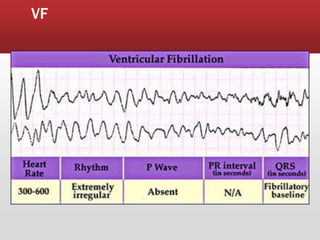
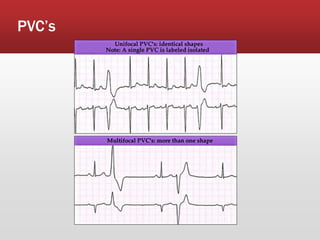
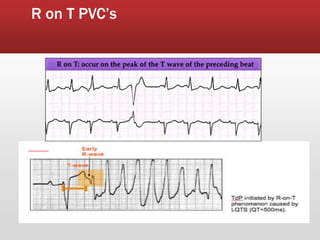
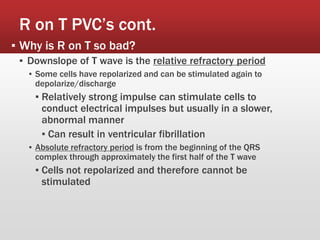
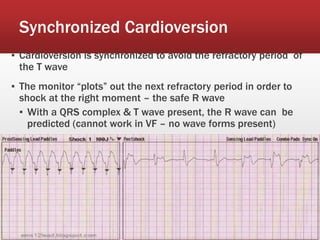
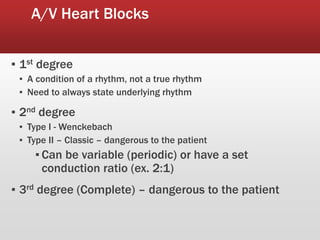
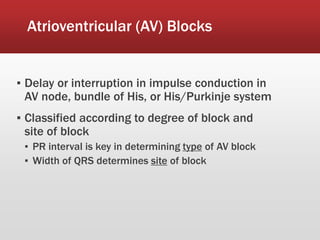
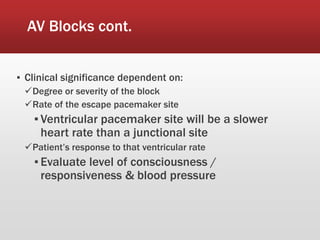
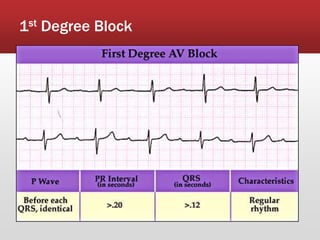
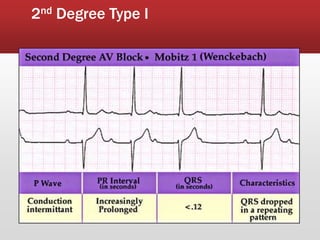
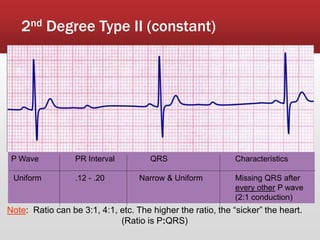
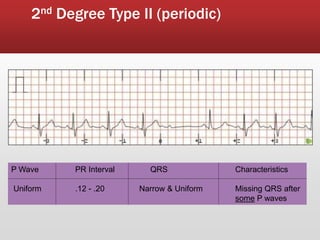
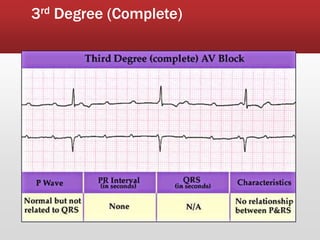
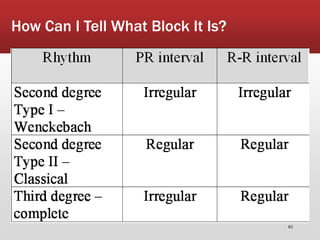
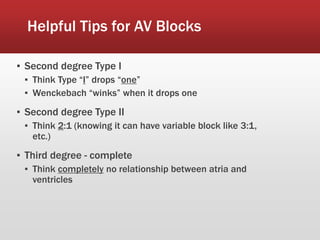
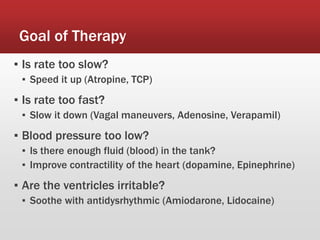
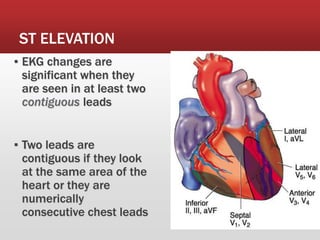
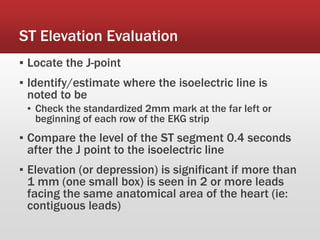
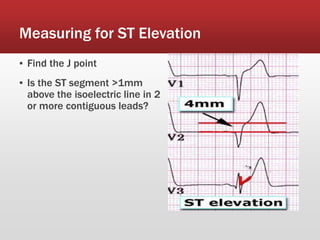
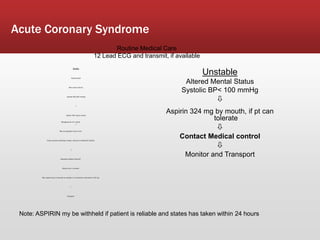
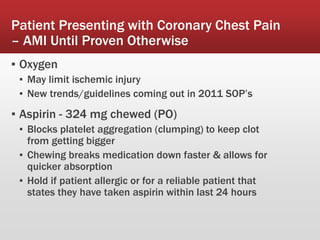
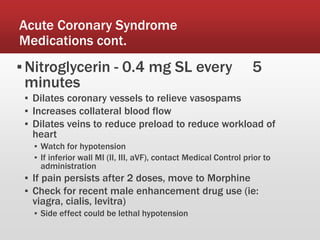
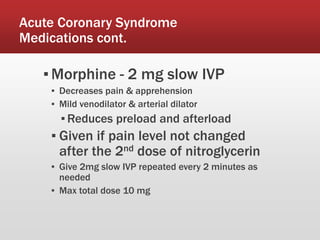
The document discusses the early detection of lethal arrhythmias and the interpretation of ECG changes, explaining the electrical activities of the heart during depolarization and repolarization. It details the components of the ECG, including waves and intervals, as well as different rhythms and heart blocks, emphasizing the clinical significance of each and their management in acute coronary syndrome. Treatment protocols for various arrhythmias and the importance of monitoring and patient evaluation are also highlighted.