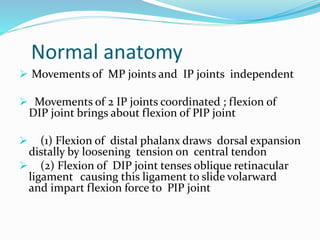
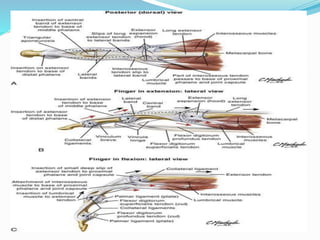
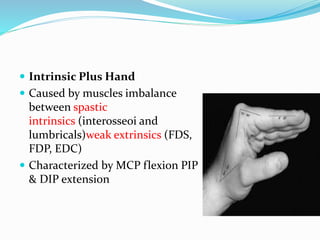
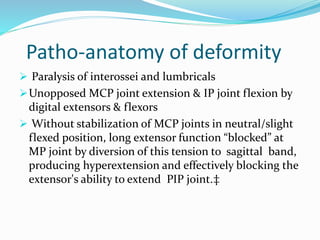
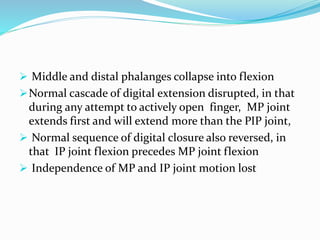
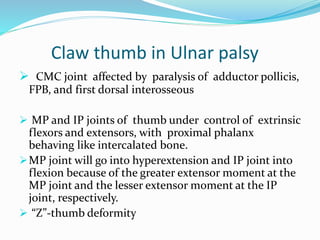
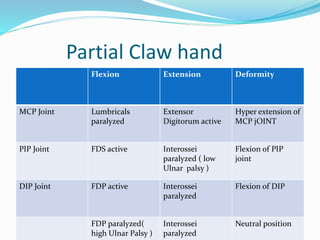
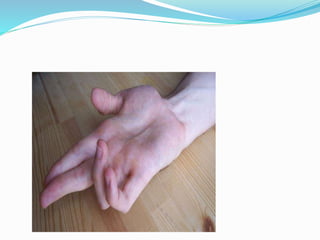
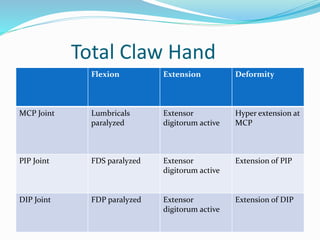
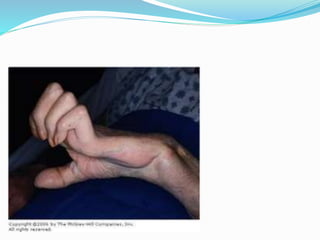
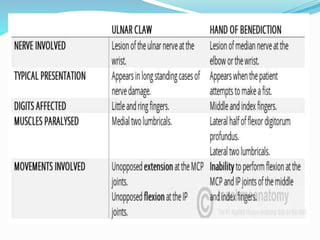
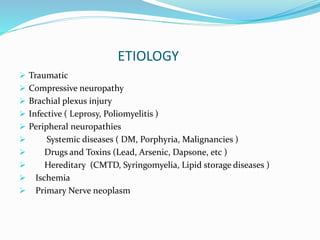
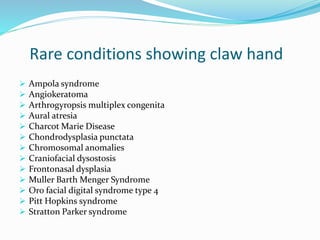
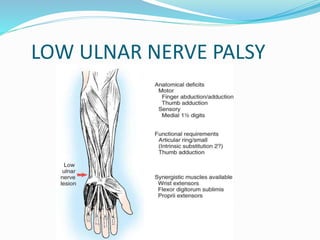
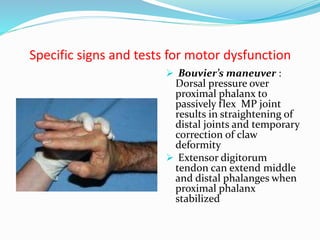
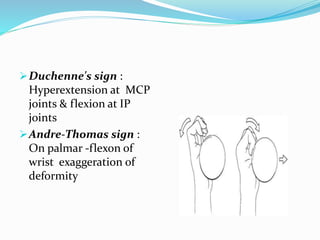
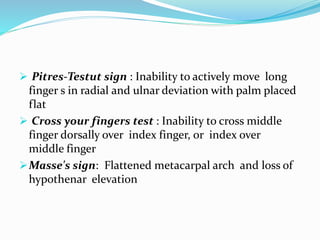
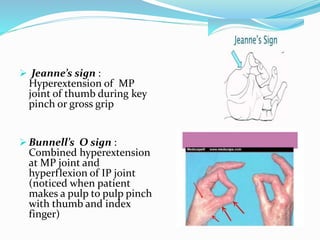
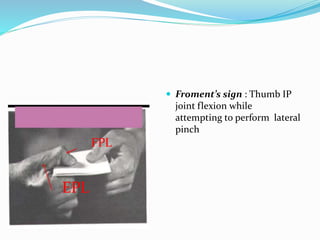
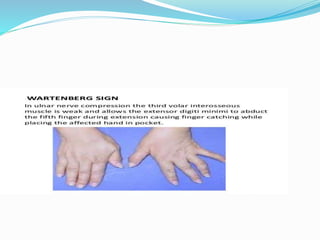
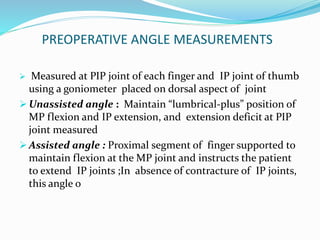
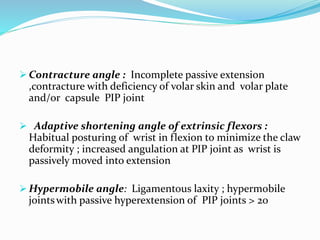
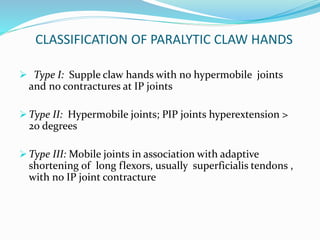
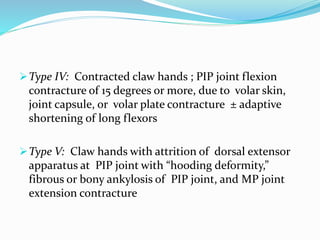
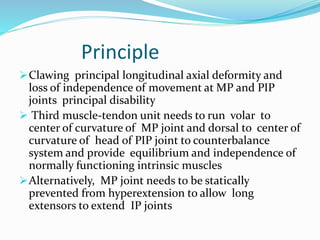
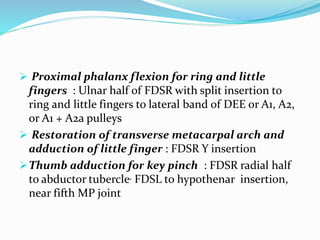
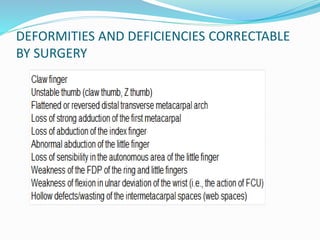
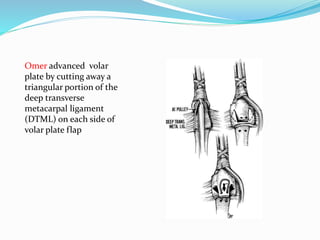
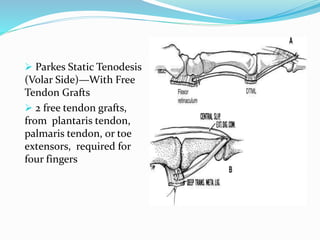
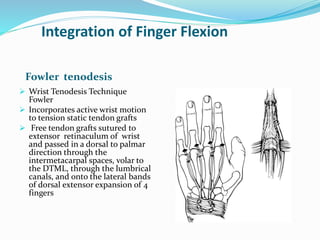
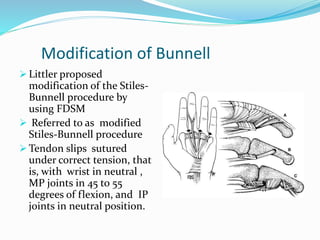
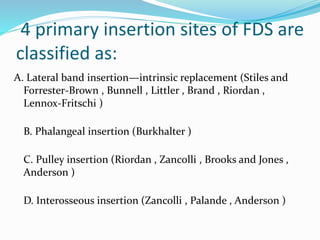
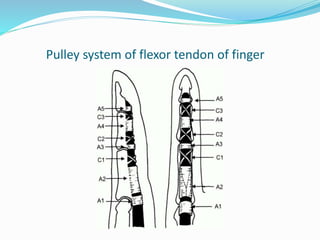
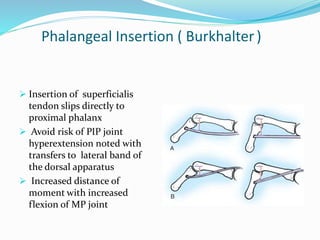
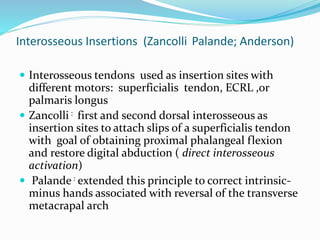
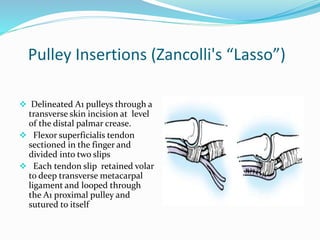
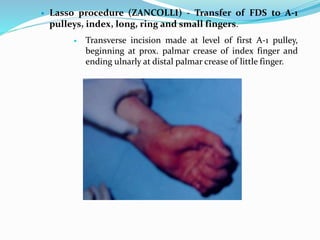
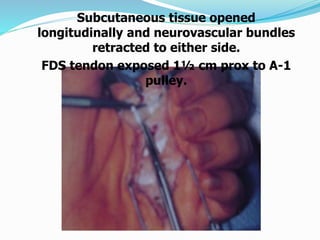
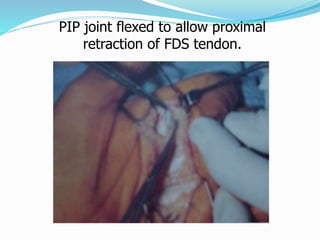
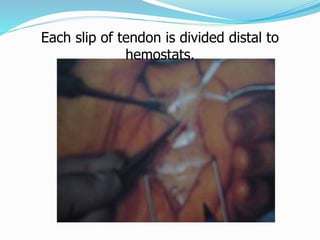
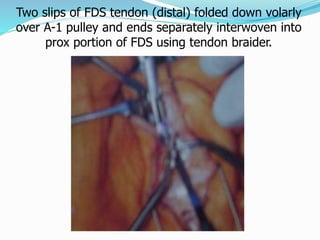
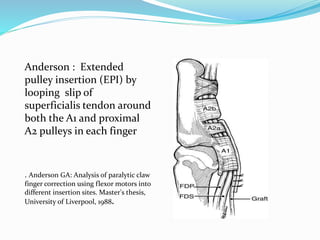
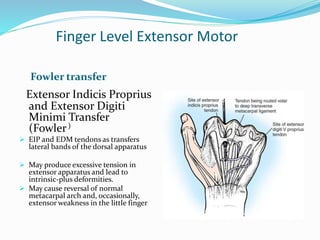
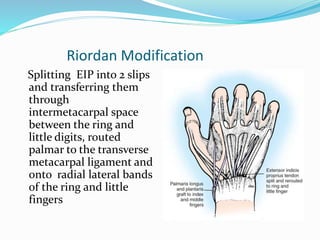
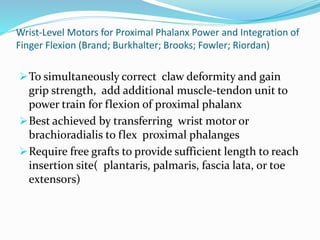
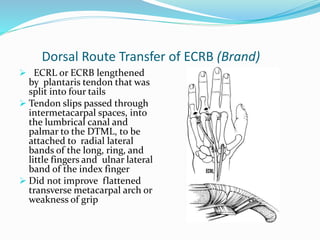
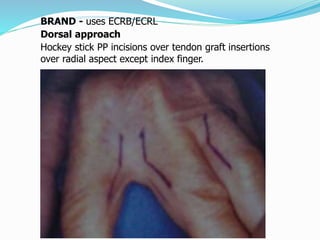
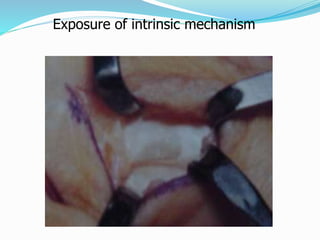
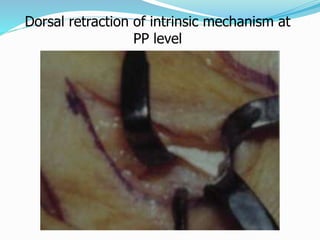
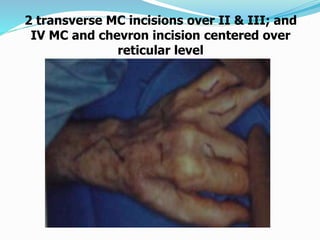
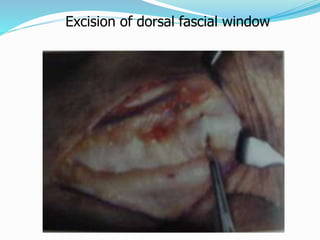
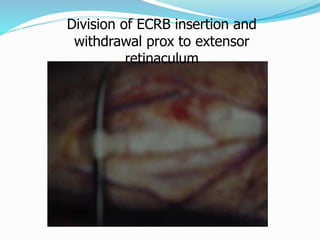
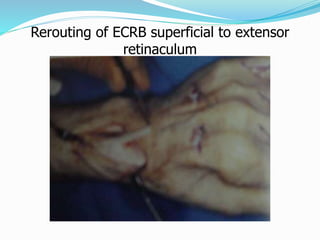
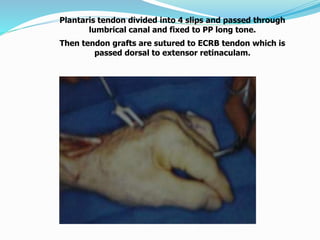
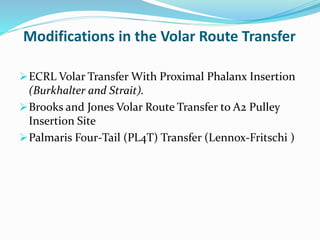
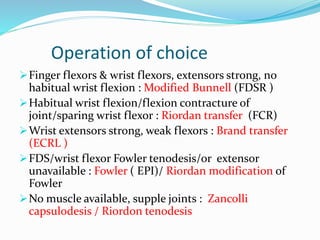
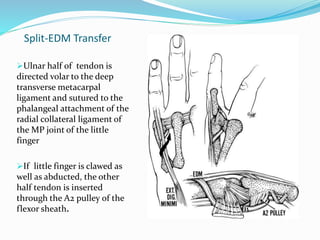
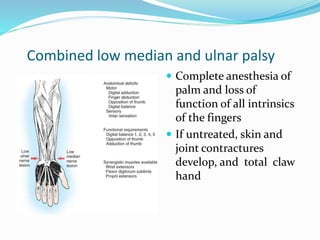
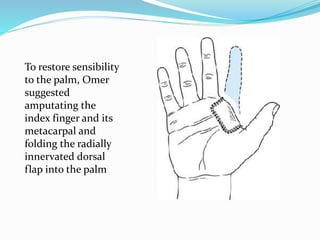
This document provides information on claw hand deformities, including definitions, anatomy, classifications, evaluation, and surgical reconstruction techniques. It begins with defining claw hand as a flattening of the transverse metacarpal arch with hyperextension of the MCP joints and flexion of the PIP and DIP joints. It then discusses the anatomy and biomechanics involved in normal versus paralytic claw hands. Various classification systems for claw hands are presented based on etiology, pattern of nerve injury, degree of involvement, and physical characteristics. Evaluation techniques such as specific tests and angle measurements are outlined. Both static and dynamic surgical reconstruction methods are then described in detail, including tendon transfers, capsulotomies, and tenode