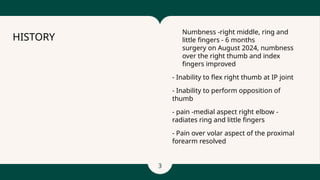
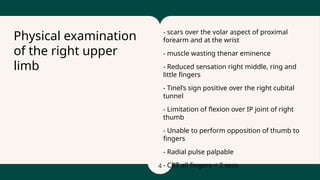
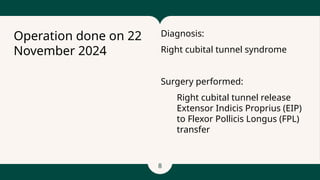
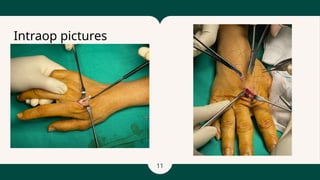
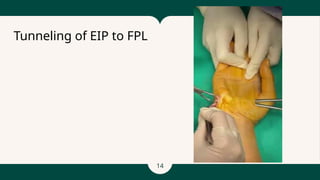
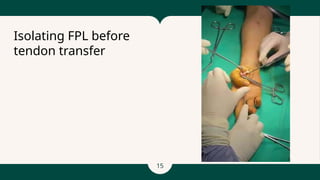
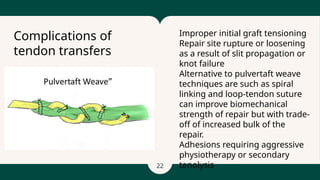
The document describes the medical history and surgical procedures performed on a 53-year-old Chinese woman suffering from right cubital tunnel syndrome, including a releasing surgery and tendon transfer to improve functionality. Operative findings highlighted the need for decompression of the ulnar nerve and the use of the extensor indicis proprius tendon to restore flexion in the thumb. Post-operative rehabilitation phases are outlined, emphasizing gradual increase of activity and strengthening exercises to enhance hand function.