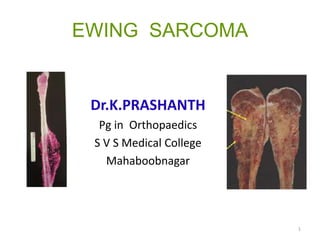
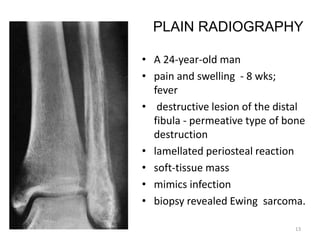
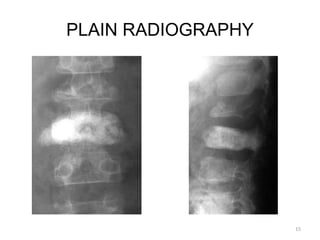
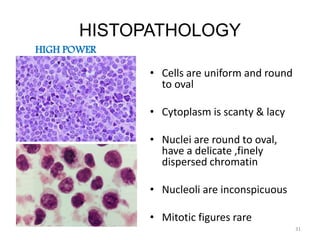
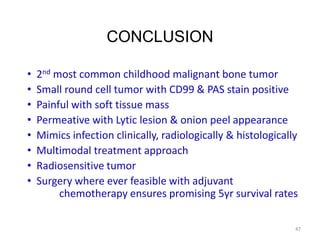
Ewing sarcoma is a highly malignant bone tumor that most commonly affects children and young adults. It is characterized by small, round cancer cells of unknown origin that invade bone and sometimes spread to soft tissues or other bones. Diagnosis involves imaging tests and biopsy showing the characteristic cells. Treatment typically involves chemotherapy, surgery to remove the tumor if possible, and sometimes radiation therapy. While Ewing sarcoma has a poor prognosis if untreated, multidisciplinary treatment with chemotherapy, surgery, and radiation can result in 5-year survival rates of 60-75% for patients without metastasis at diagnosis.