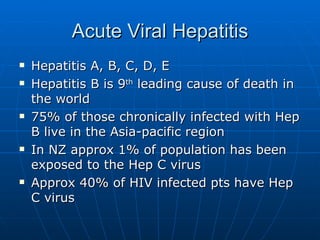
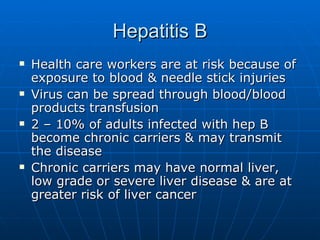
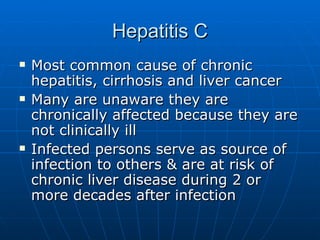
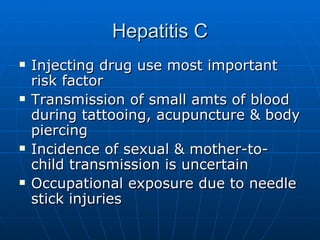
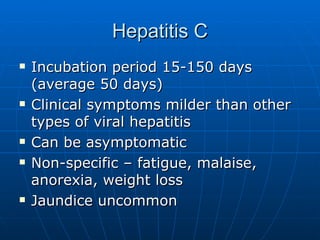
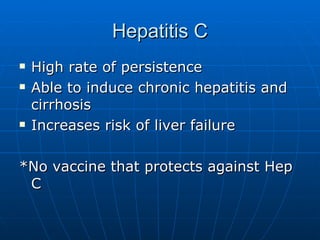
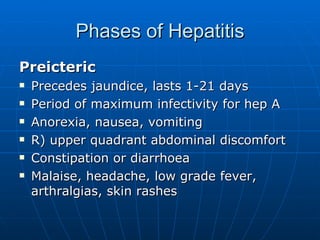
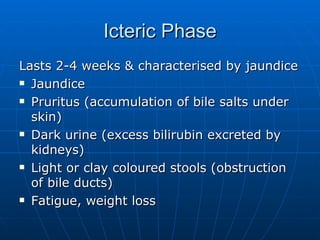
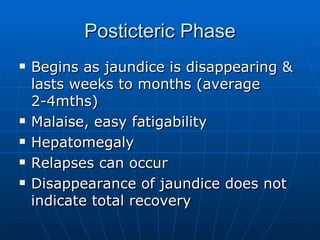
The document discusses hepatitis, which is inflammation of the liver. It outlines the various causes of hepatitis including viruses, chemicals, drugs, and autoimmune diseases. It focuses on the different types of viral hepatitis (A, B, C, D, E), their symptoms, modes of transmission, risks, and ability to cause both acute and chronic conditions. Hepatitis B and C are particularly discussed as leading causes of chronic liver disease and liver cancer worldwide.