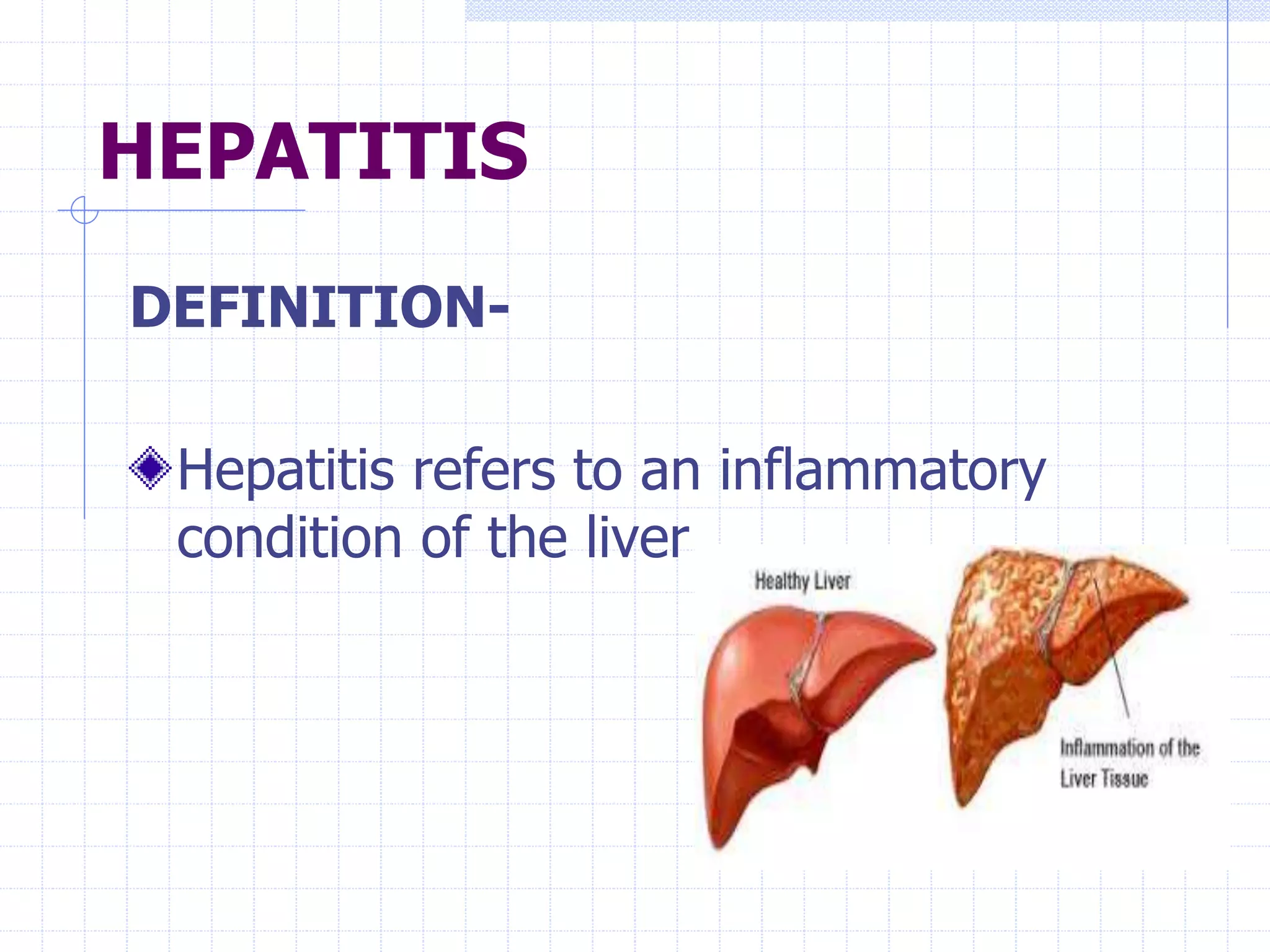
This document provides information about jaundice and hepatitis. It begins with an introduction to jaundice, defining it as a yellowish discoloration of the skin and eyes caused by elevated bilirubin levels. It then discusses the causes, signs, and types of jaundice, including hemolytic, hepatocellular, and obstructive jaundice. The document also covers hepatitis A-E, describing the viruses, transmission, prevention, and treatment of each type. It concludes with a discussion of liver anatomy and function, jaundice diagnosis and management, and nursing care for patients with jaundice or hepatitis.