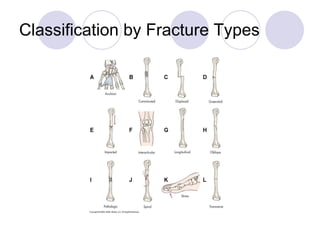
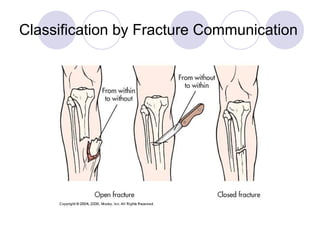
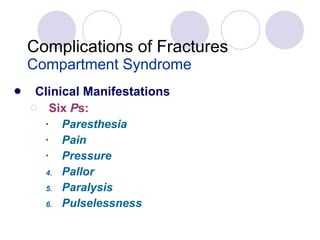
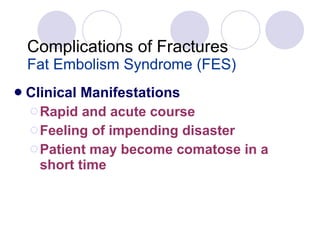
This document describes fractures, including their classification, healing process, treatment methods, and potential complications. Fractures are breaks in bone continuity that can be open or closed. Treatment involves reduction, immobilization with casts or devices, and monitoring for complications like infection, compartment syndrome, blood clots, and fat embolism syndrome. Fracture healing is a multi-stage process of hematoma formation, new tissue growth, callus formation, bone consolidation and remodeling over several weeks or months.