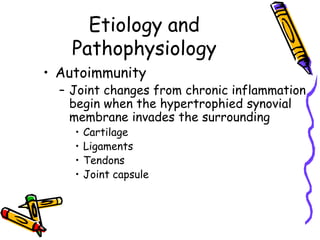
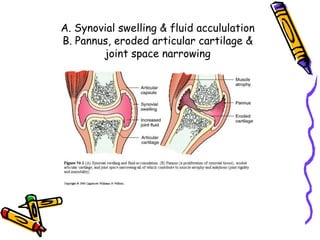
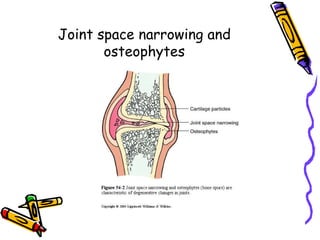
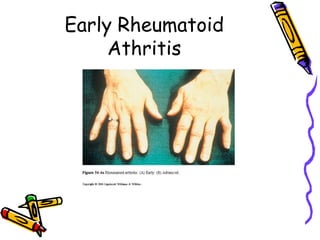
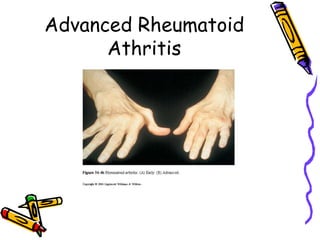
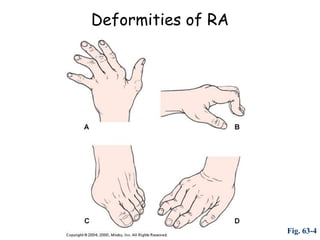
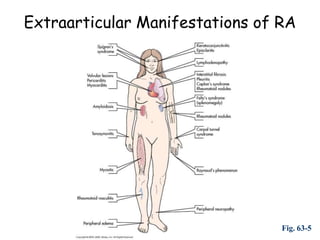
Rheumatoid arthritis is a chronic autoimmune disease characterized by inflammation of the synovial joints. It affects all ethnic groups and can occur at any time in life, though incidence increases with age and it is more common in women. While the specific cause is unknown, it is believed to involve an abnormal immune response triggered by an antigen that leads to the formation of autoantibodies and immune complexes that damage joints. Long-term inflammation and damage to joints can cause pain, stiffness, swelling, and deformities like subluxation. It may also affect other body systems.
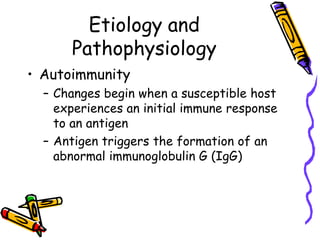
![Etiology and
Pathophysiology
• Autoimmunity
– RA is characterized by the presence of
autoantibodies (rheumatoid factor [RF])
– RF and IgG form immune complexes that
initially deposit on synovial membranes
or superficial articular cartilage in the
joints
– An inflammatory response results](https://image.slidesharecdn.com/4rheumatoidarthriis2010-100302035148-phpapp01/85/4-Rheumatoid-Arthriis-2010-5-320.jpg)