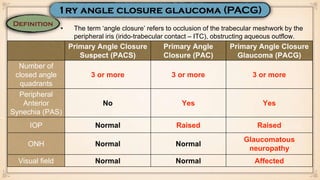
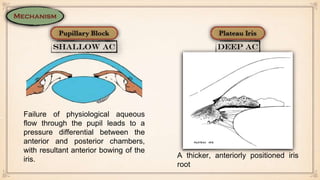
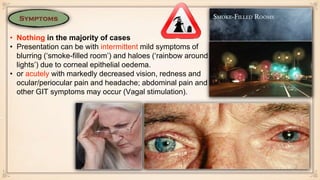
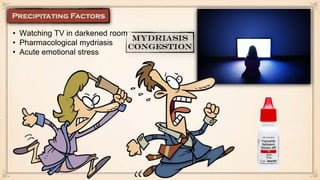
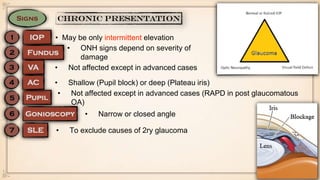
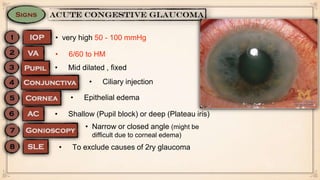
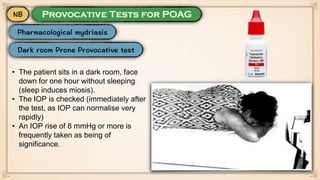
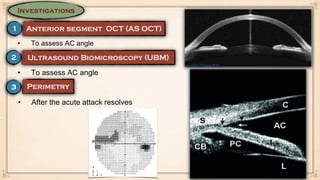
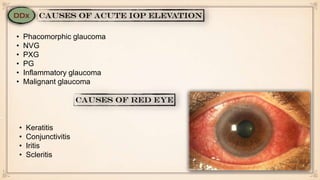
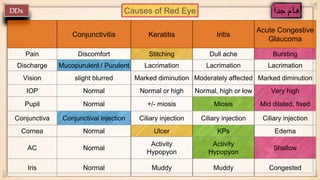
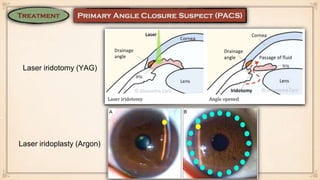
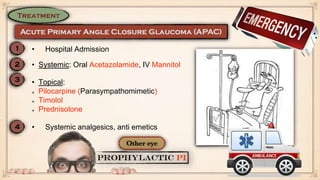
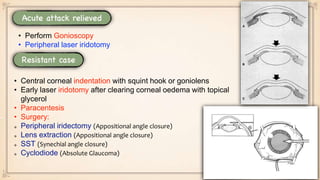
This document discusses different types of angle closure conditions including primary angle closure suspect (PACS), primary angle closure (PAC), and primary angle closure glaucoma (PACG). It provides details on diagnosis, risk factors, symptoms, examination findings, treatment options including laser iridotomy, and management of acute angle closure attacks.