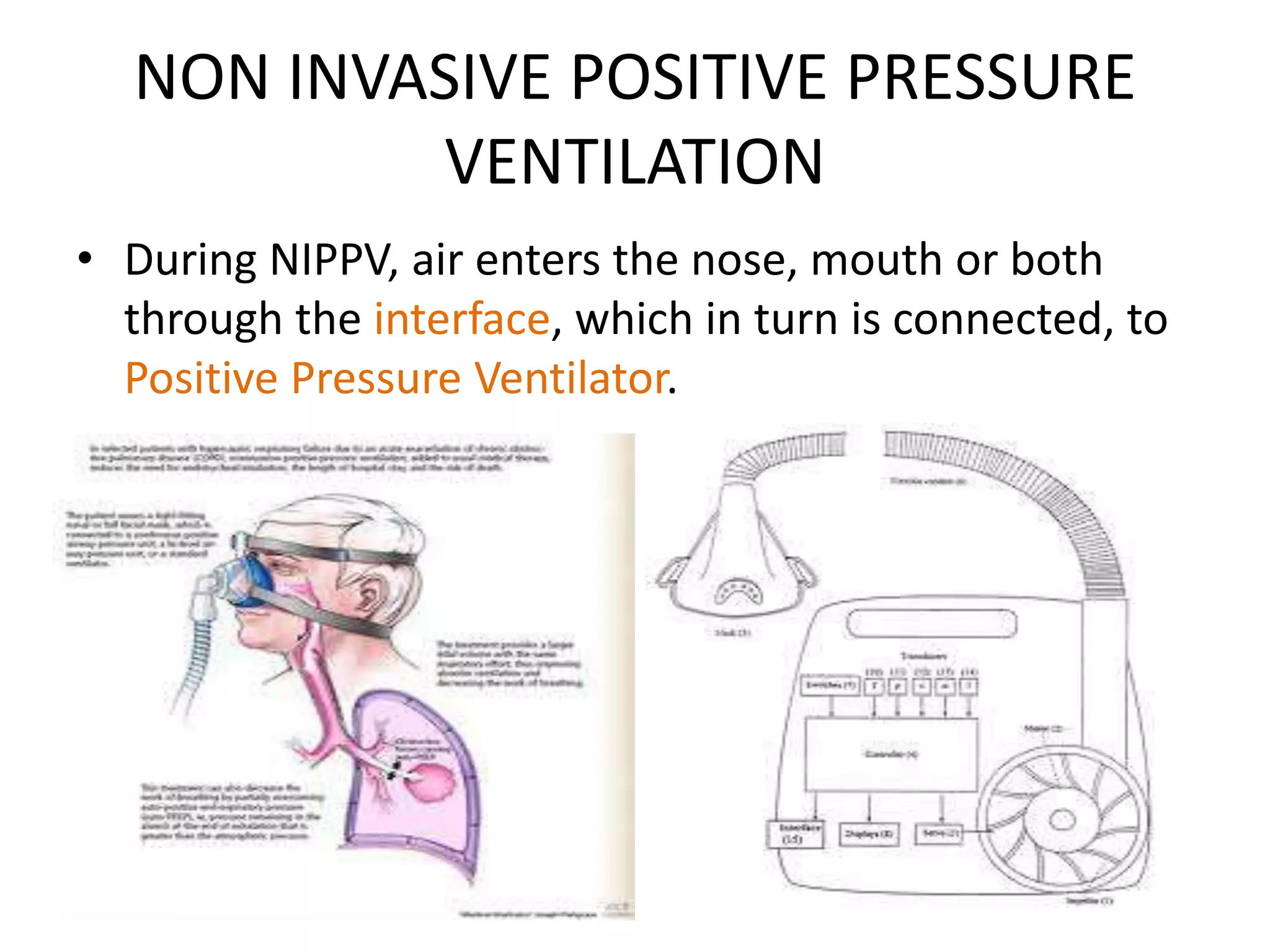
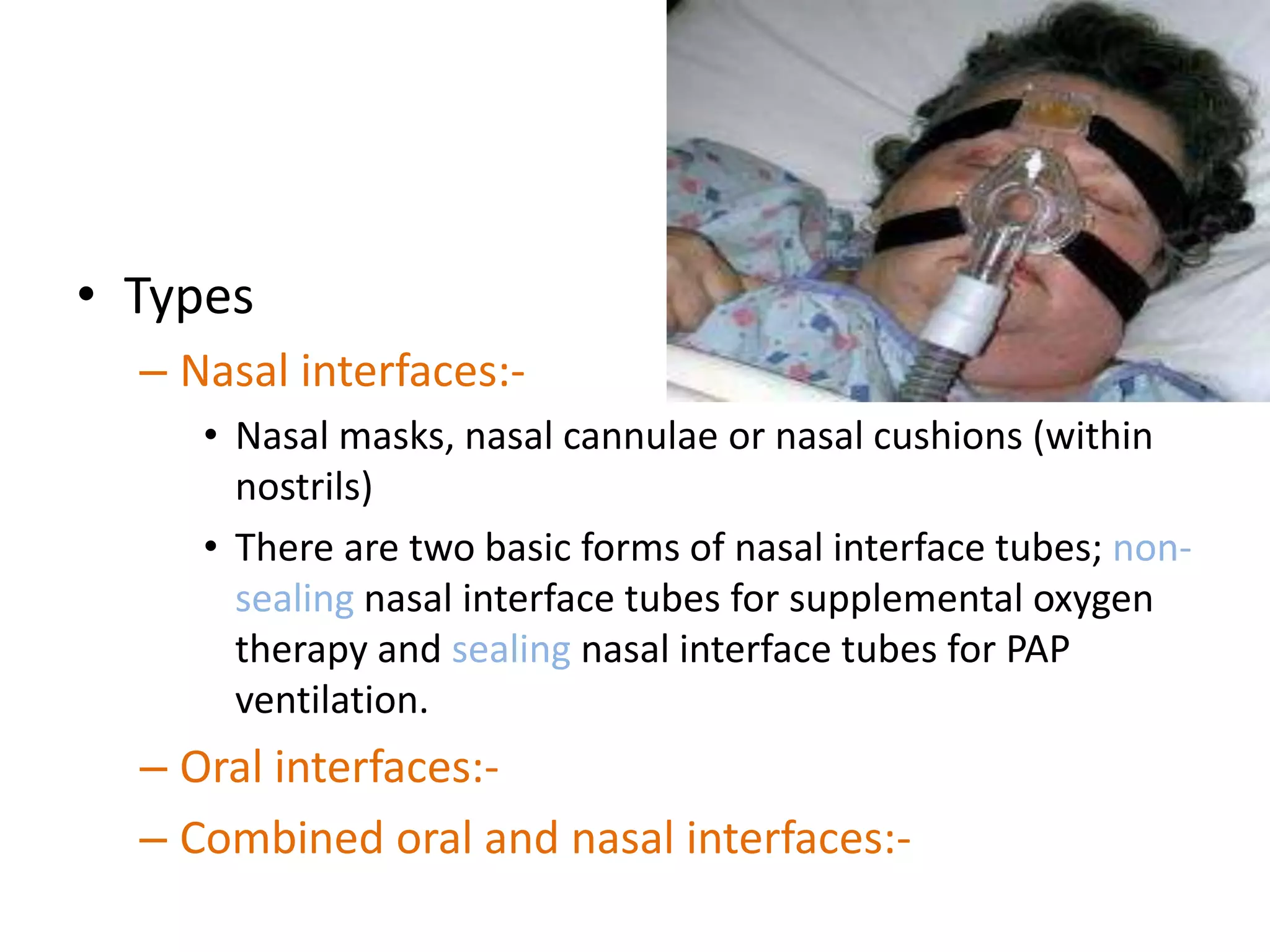
Non-invasive ventilation (NIV) delivers respiratory support without invasive airway procedures, with historical developments dating back to the 19th century. It includes techniques like non-invasive positive pressure ventilation and negative pressure ventilation, offering advantages such as reduced complications and improved patient comfort, but also comes with risks like air leaks and mask discomfort. Successful NIV requires patient cooperation and specific monitoring criteria, with indications for use ranging from acute respiratory failure to chronic respiratory conditions.