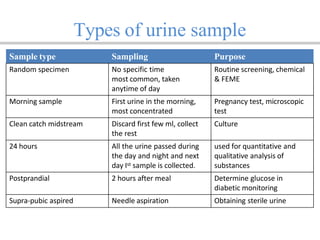
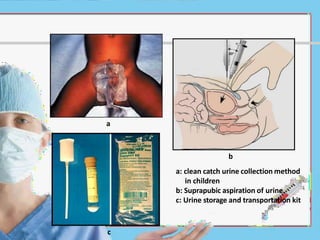
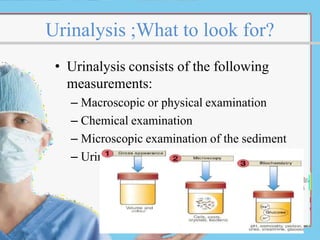
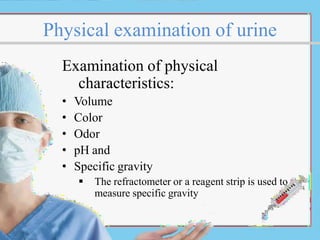
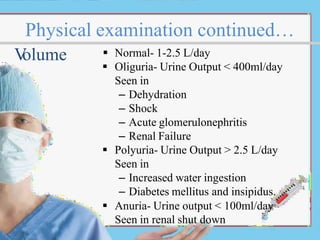
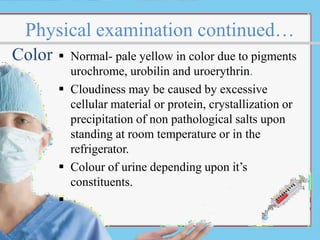
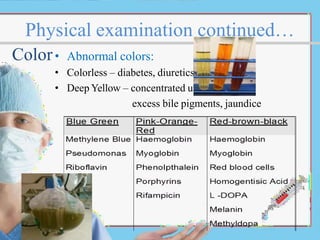
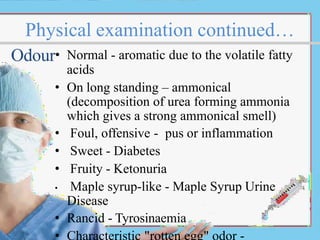
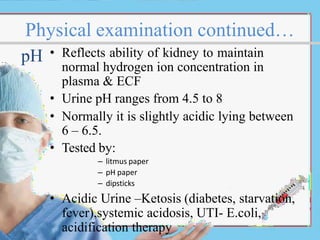
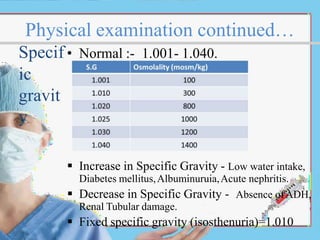
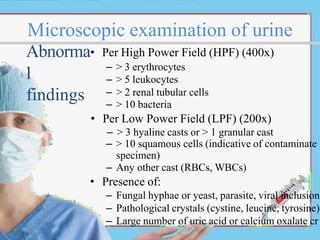
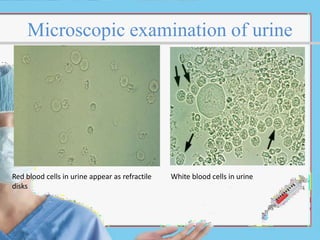
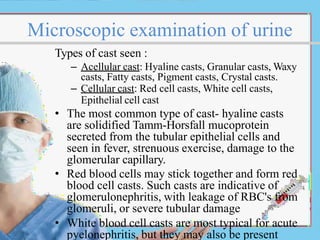
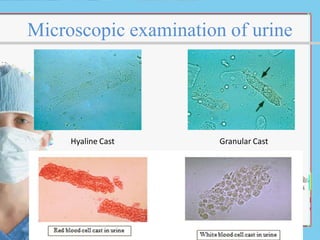
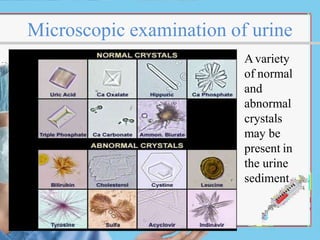
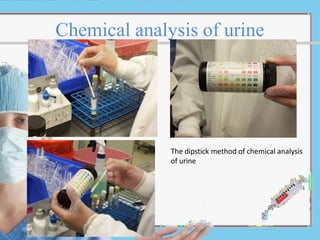
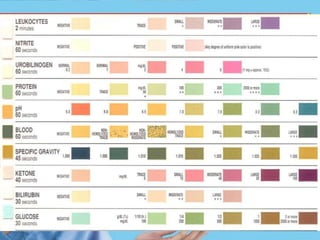
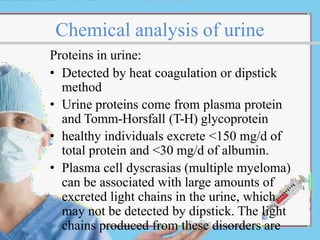
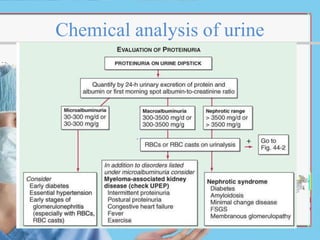
Urine analysis, also called urinalysis, is one of the oldest medical laboratory procedures. It involves physical, chemical, and microscopic examination of urine samples to evaluate health, diagnose diseases of the kidneys or urinary tract, and monitor certain medical conditions like diabetes. Proper collection and handling of urine specimens is important for valid test results. A urinalysis provides information on various physical characteristics of urine like color, odor, pH, and specific gravity. Under the microscope, urine sediment is examined for abnormalities like blood, protein, casts, crystals, and bacteria. Chemical analysis with dipstick testing detects substances like protein, glucose, ketones, blood, and other electrolytes. Together, the different components of a urinal