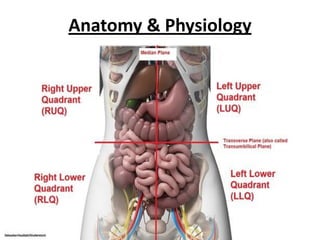
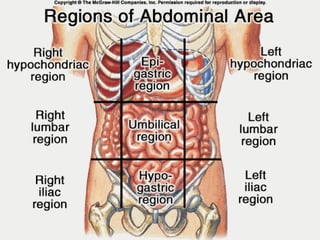
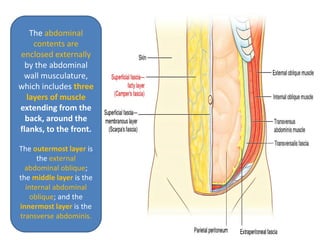
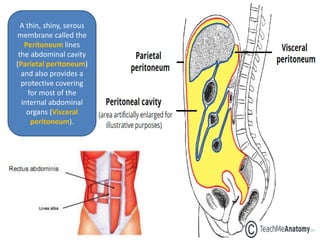
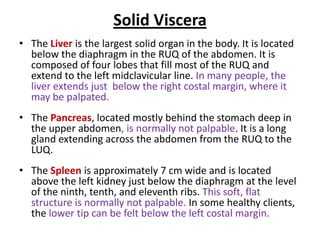
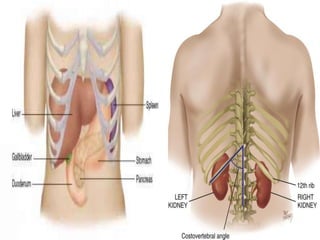
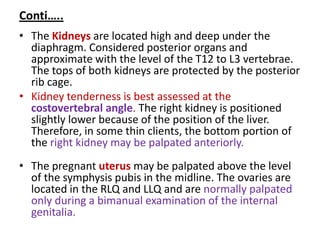
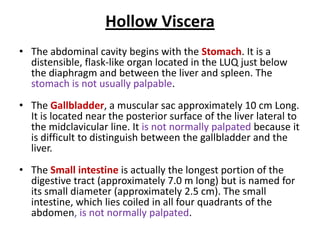
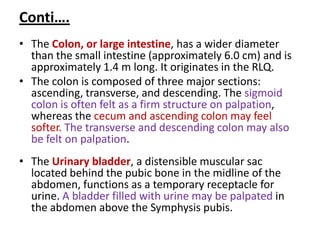
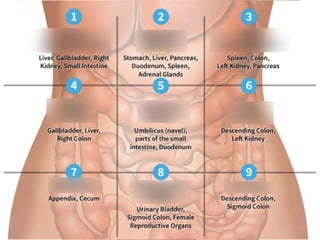
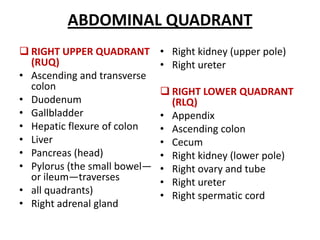
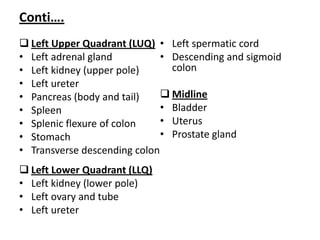
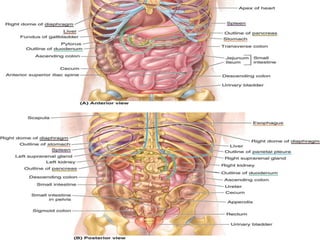
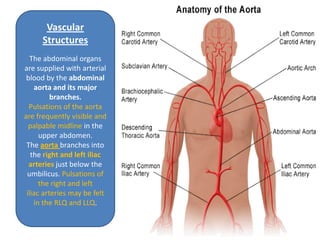
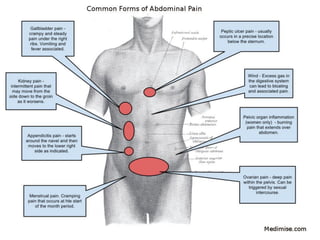
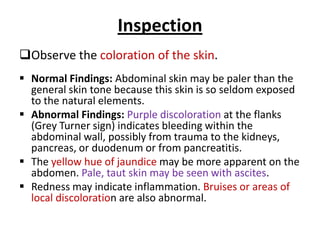
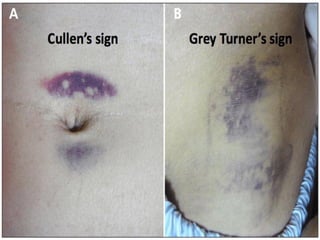
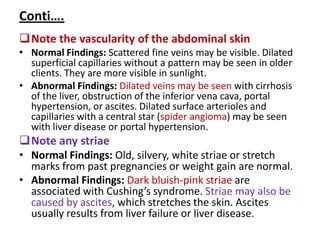
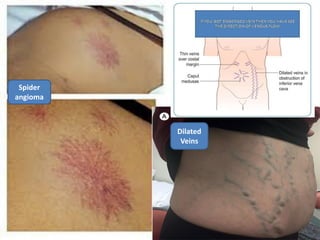
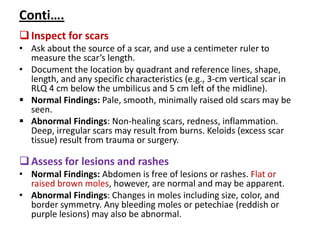
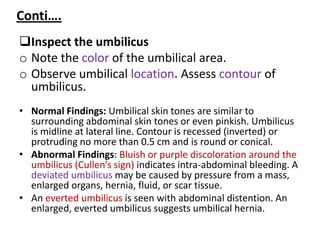
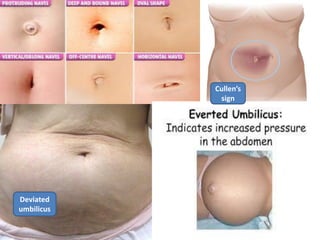
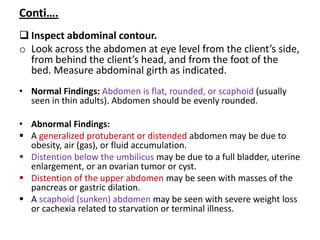
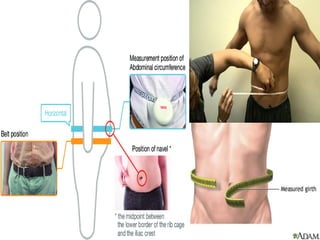
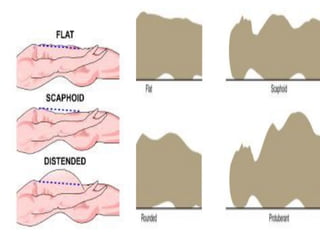
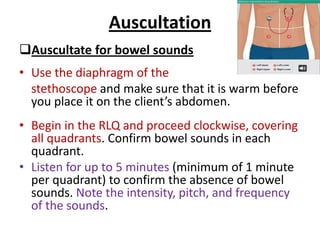
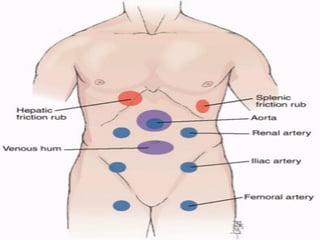
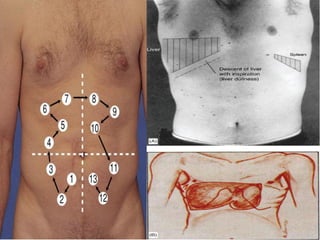
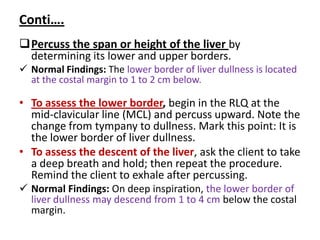
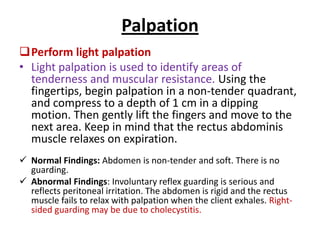
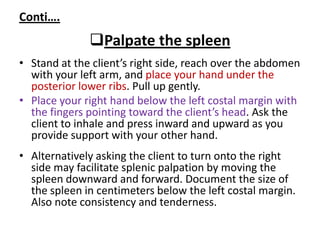
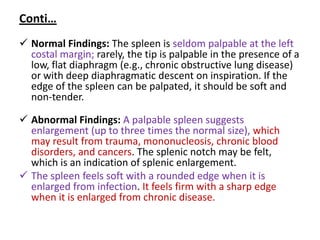
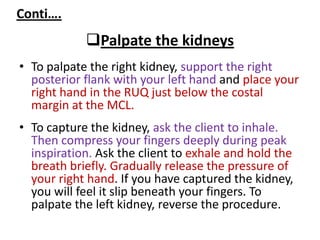
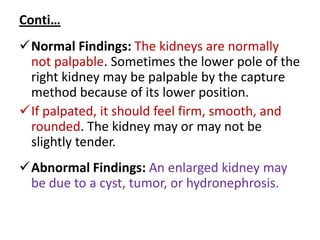
This document provides information about performing a physical examination of the abdomen. It describes the anatomy of the abdominal wall and contents. The peritoneum lines the abdominal cavity. Structures within the cavity include solid organs like the liver and hollow organs like the stomach. The document outlines the steps of inspecting, auscultating, and palpating the abdomen and defines normal and abnormal findings for each step.