This document discusses fluid and electrolyte balance in surgery. It covers:
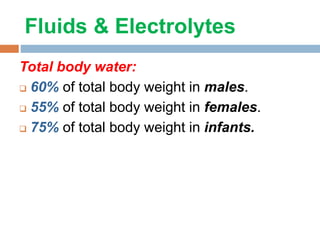
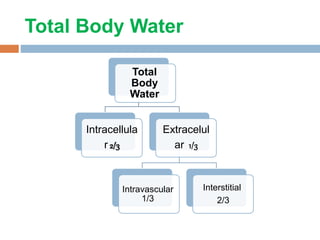
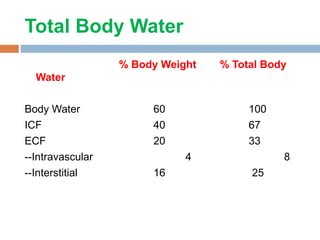
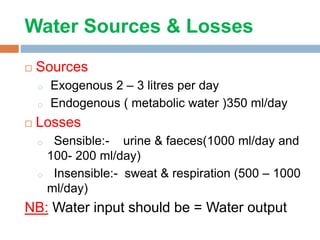
1. Total body water distribution, with most being intracellular. Fluid sources and losses are discussed.
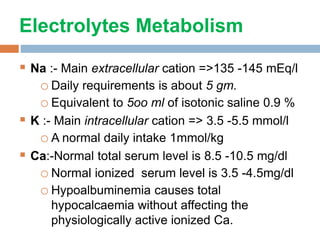
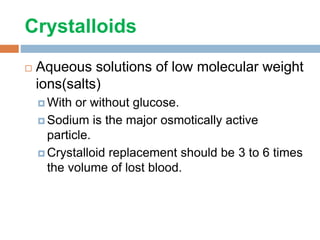
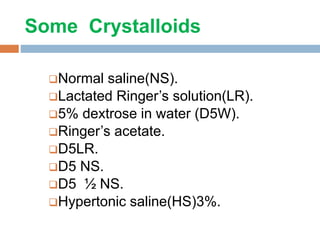
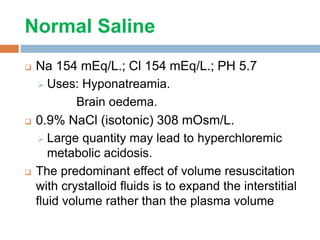
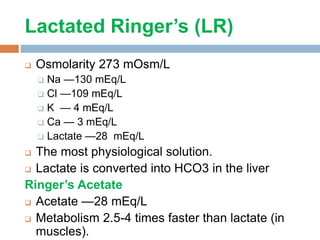
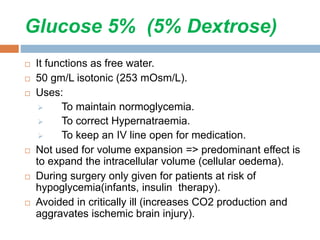
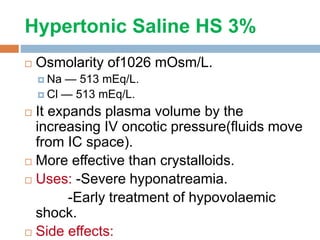
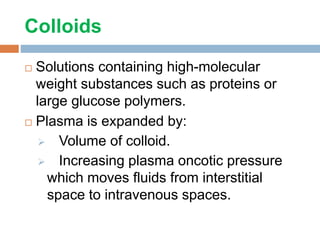
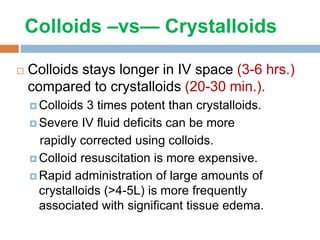
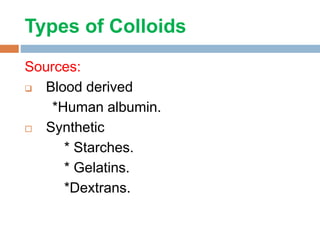
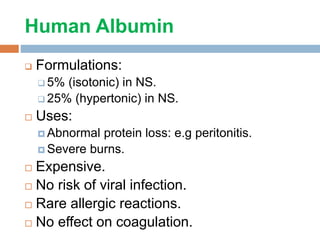
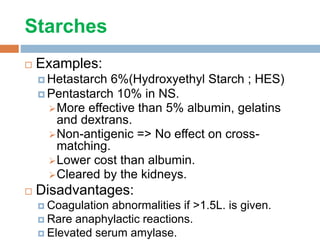
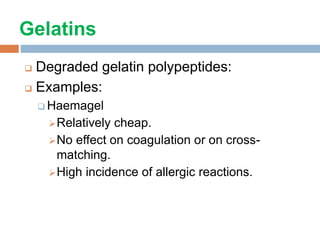
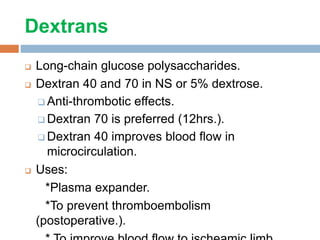
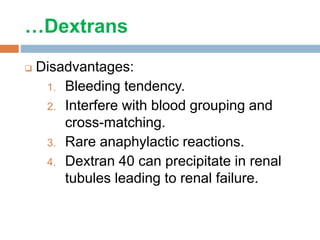
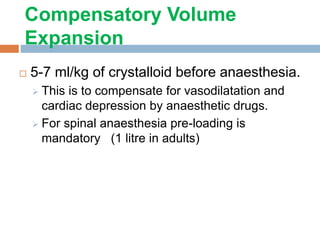
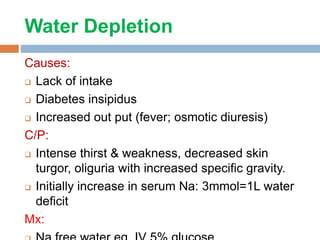
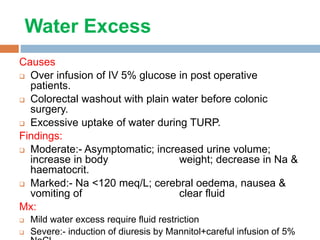
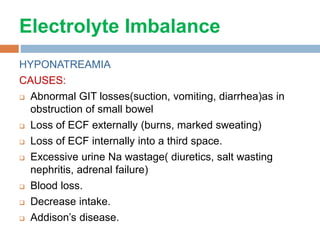
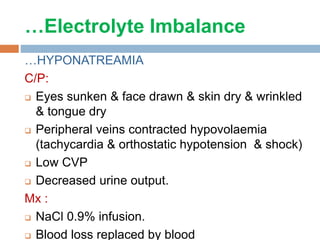
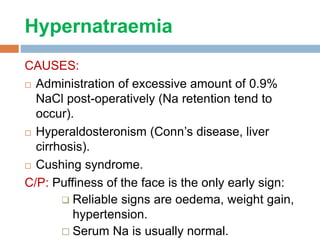
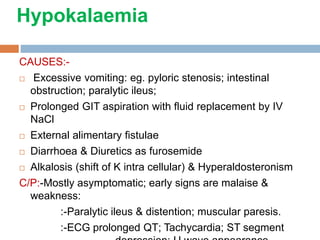
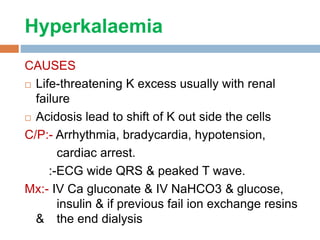
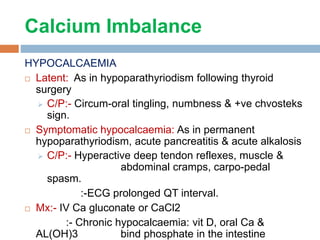
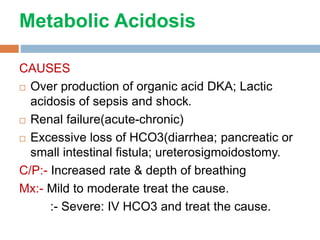
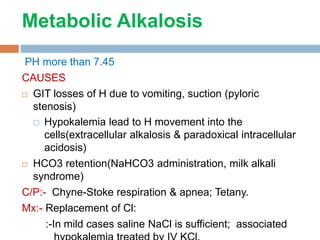
2. Electrolytes like sodium, potassium, and calcium are important to maintain balance of. Crystalloid and colloid fluids are compared for volume expansion abilities.
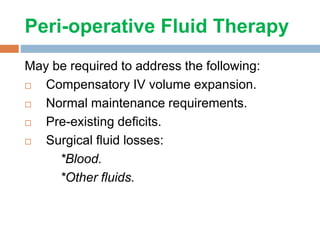
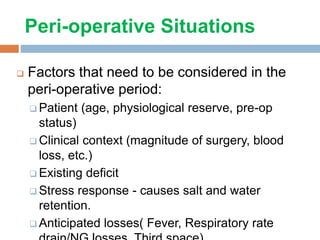
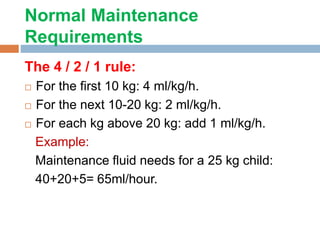
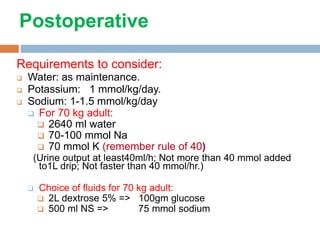
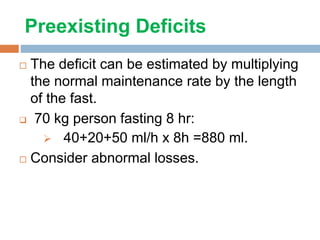
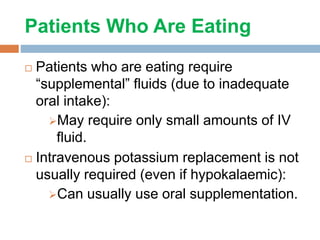
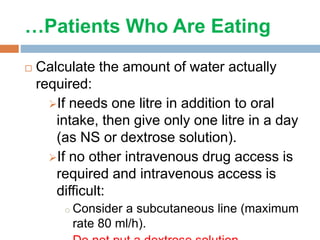
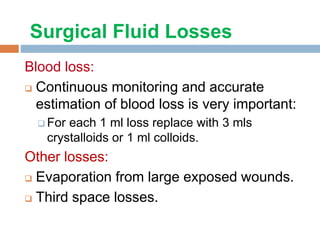
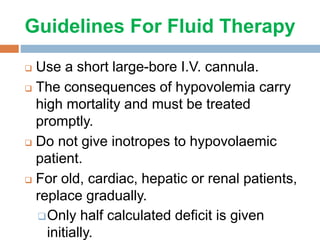
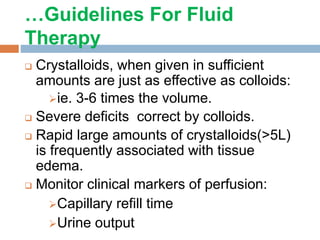
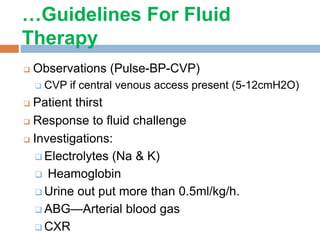
3. Perioperative fluid therapy aims to maintain normovolemia, electrolyte balance, and blood sugar. Fluid types, deficits, and losses are factors to consider for therapy. Guidelines emphasize prompt treatment of hypovolemia and monitoring for adequacy of resuscitation.