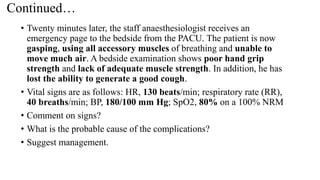
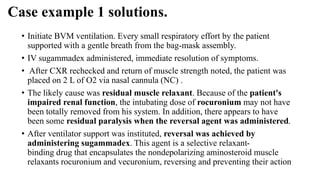
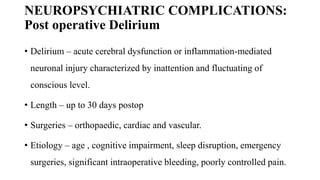
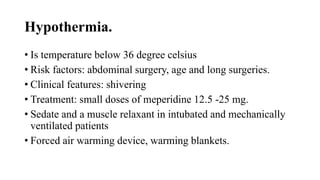
The document discusses various post-operative complications related to the cardiovascular system (CVS), central nervous system (CNS), and recovery in the post-anesthesia care unit (PACU). Some key points include: common CVS complications are hypotension and hypertension, which can be treated with fluid administration or vasopressors/antihypertensives respectively; arrhythmias are also common after cardiac surgery; common neuropsychiatric complications in PACU include delirium, delayed arousal, and failure to arouse due to various medical causes; and hypothermia is another potential complication addressed by maintaining normothermia.