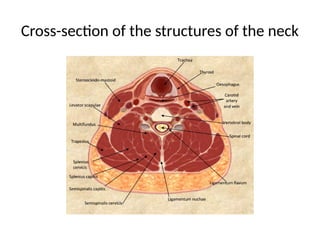
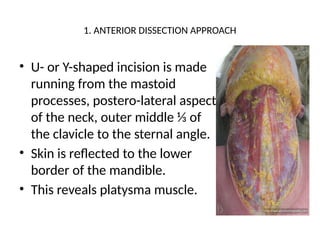
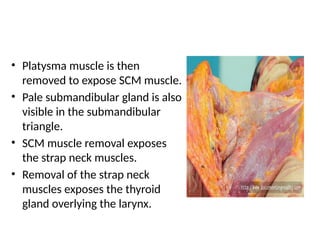
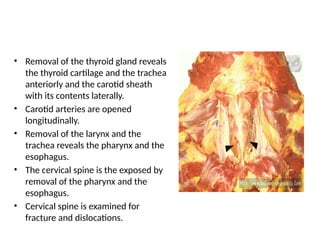
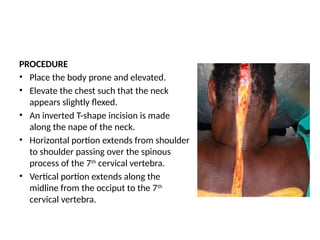
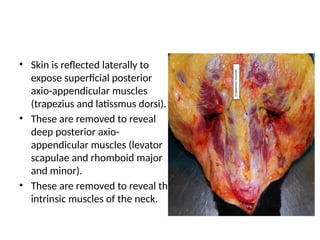
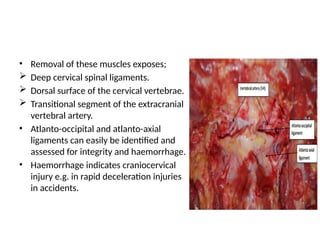
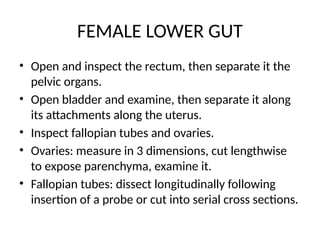
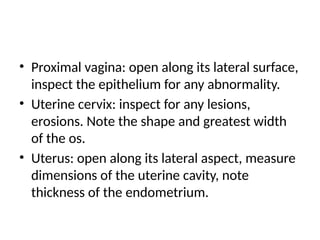
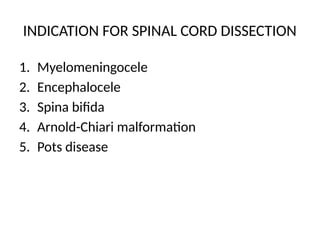
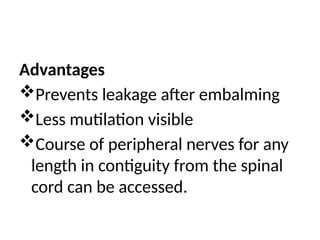
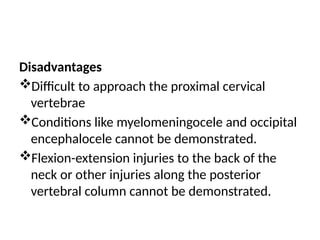
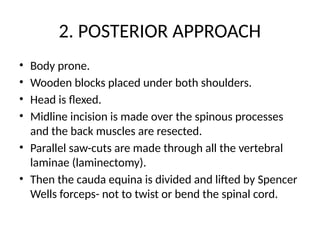
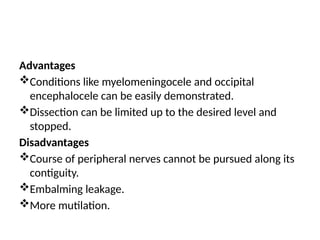
The document outlines various special dissection techniques, including neck, pelvic, spinal cord, and pediatric head dissection, detailing their indications, methods, and anatomical considerations. Each dissection type is explained with specific procedural steps and associated indications for use, such as asphyxia for neck dissection or hydrocephalus for pediatric head dissection. Techniques for minimizing hemorrhage and ensuring thorough examination are emphasized throughout the procedures.