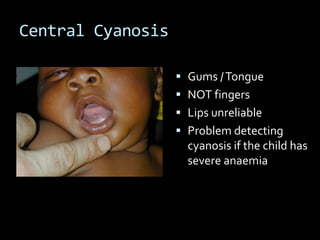
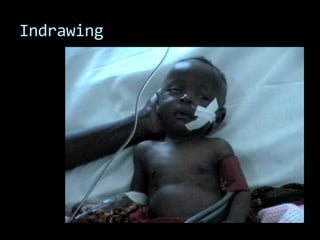
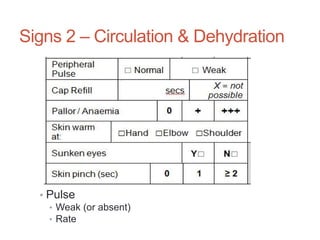
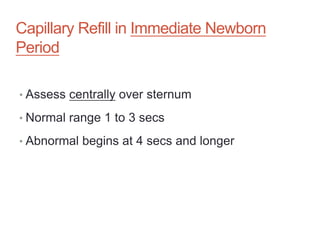
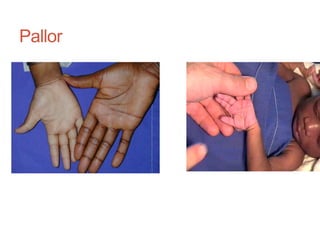
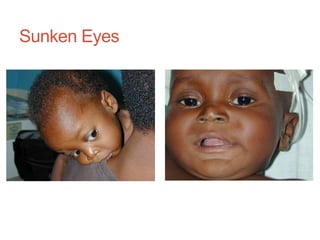
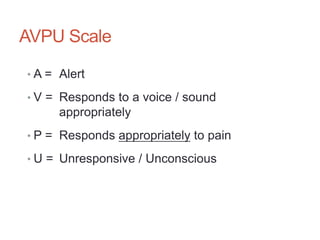
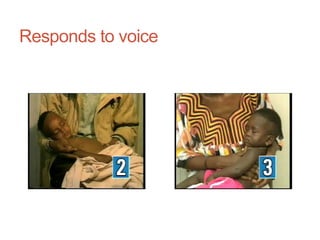
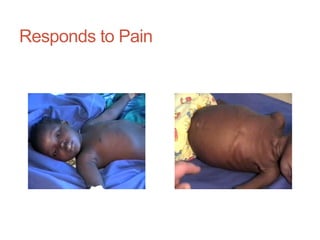
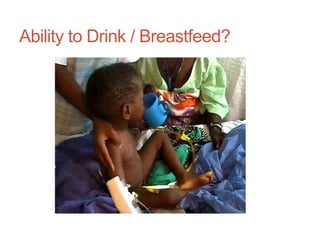
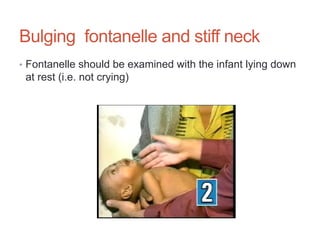
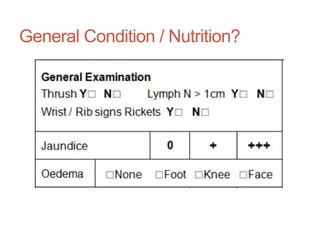
The document discusses essential clinical symptoms and signs for assessing common serious diseases. It emphasizes that the most useful symptoms and signs are those that are commonly observed in common illnesses, help evaluate the nature and severity of illness, indicate risk of death, are useful for monitoring progress, can differentiate diseases, and are easy for everyone to observe and learn. It describes choosing symptoms and signs that have a strong evidence base for the most common childhood disorders and are included in the Integrated Management of Neonatal and Childhood Illness approach.