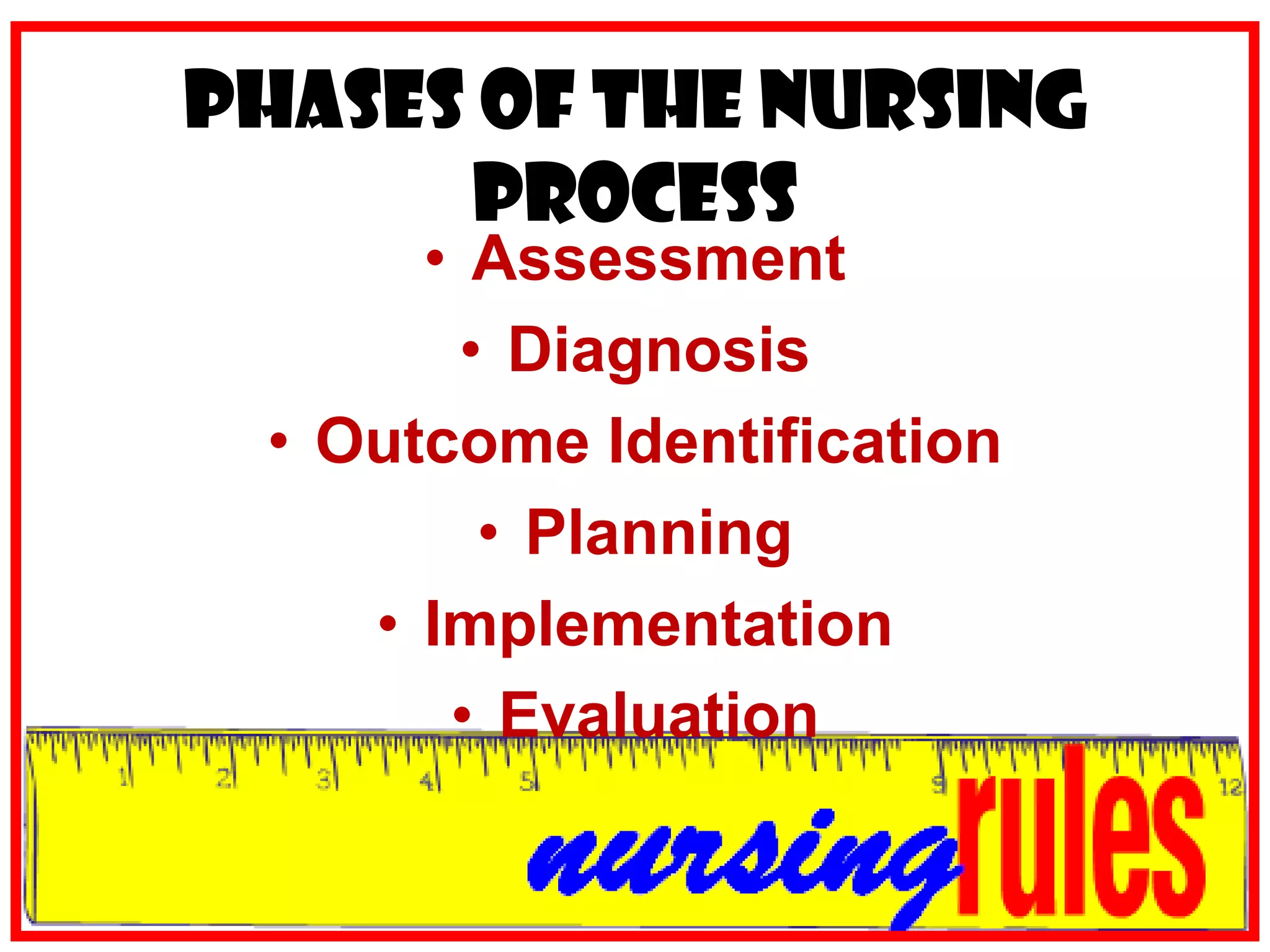
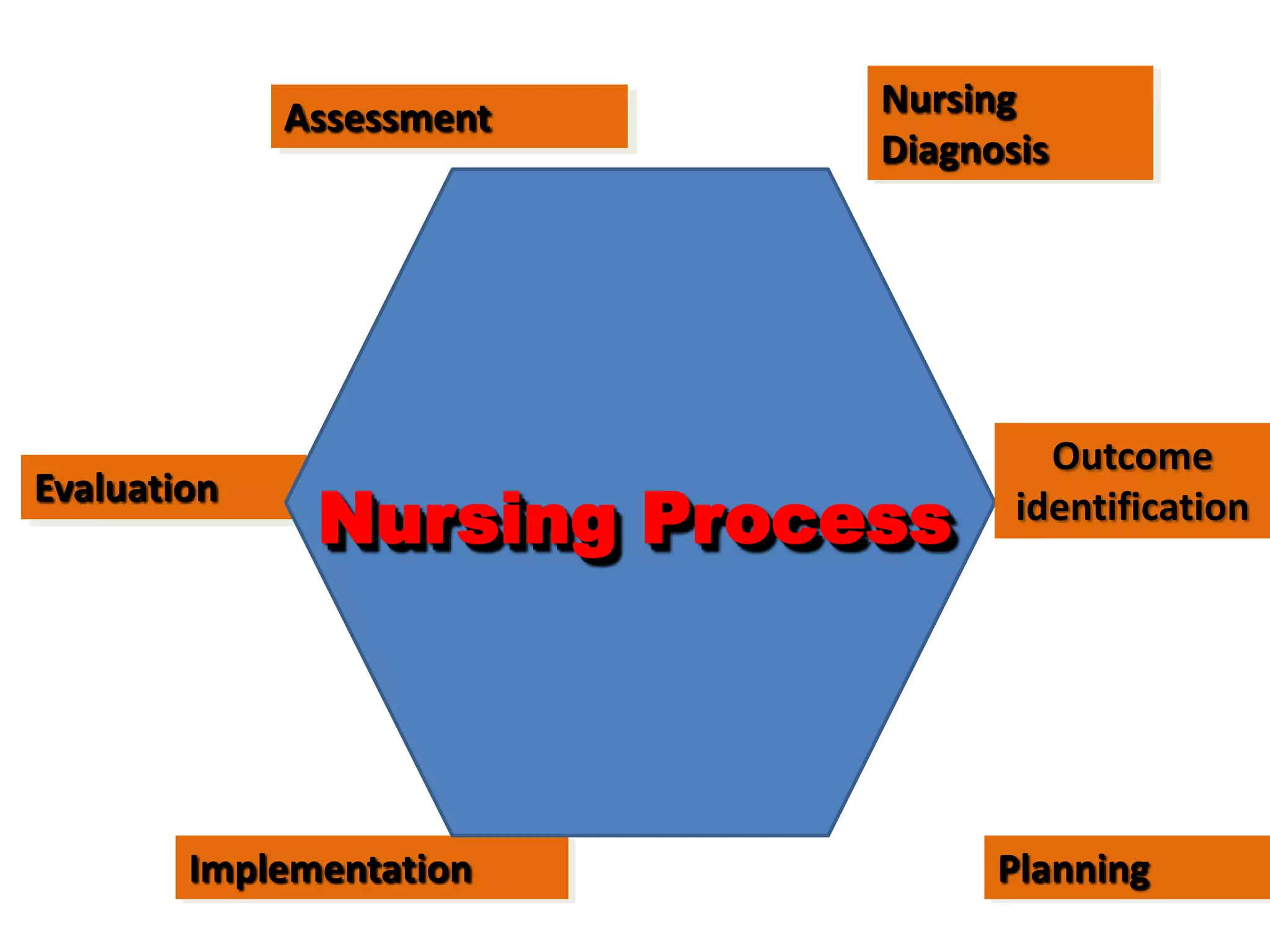
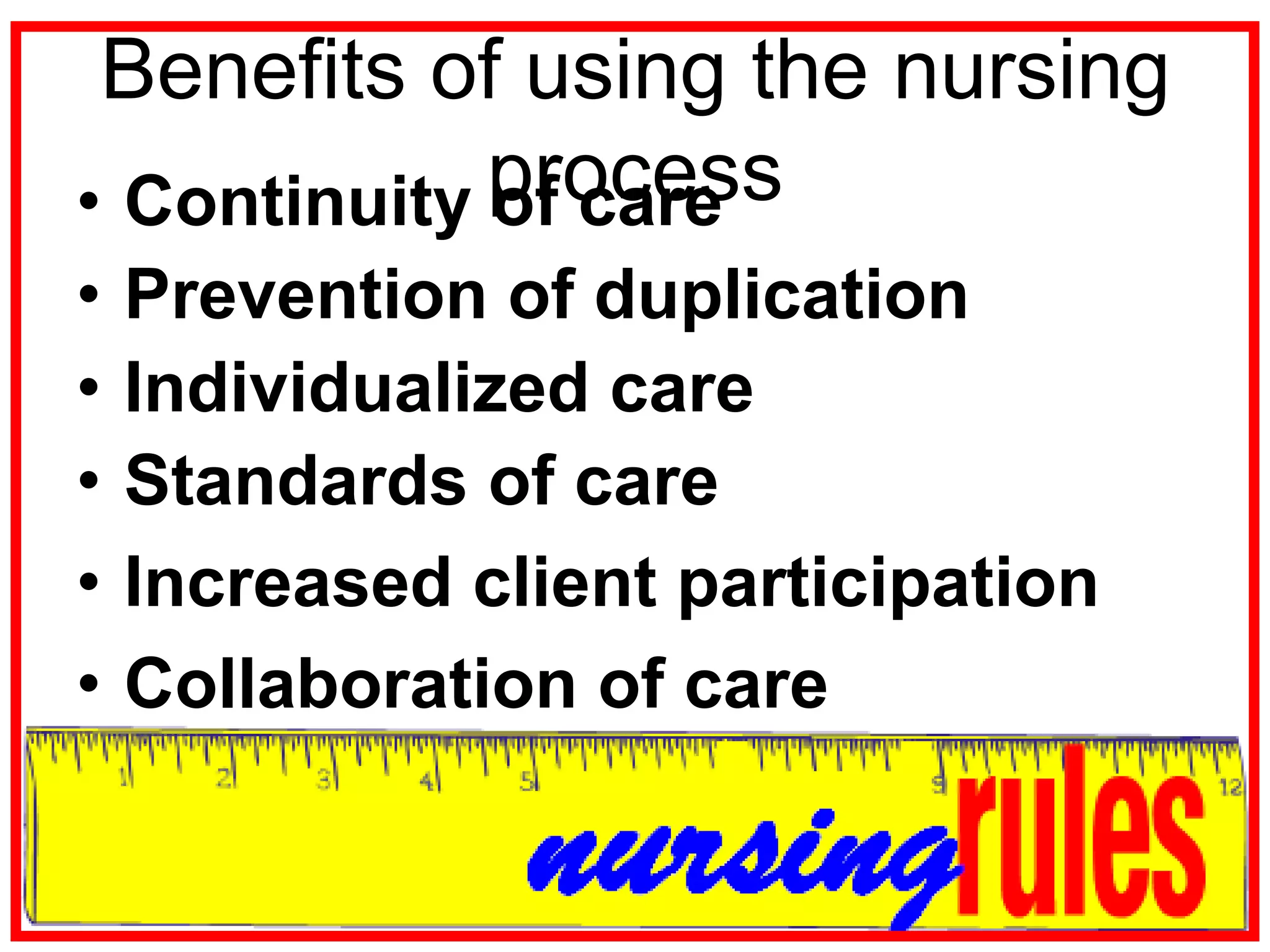
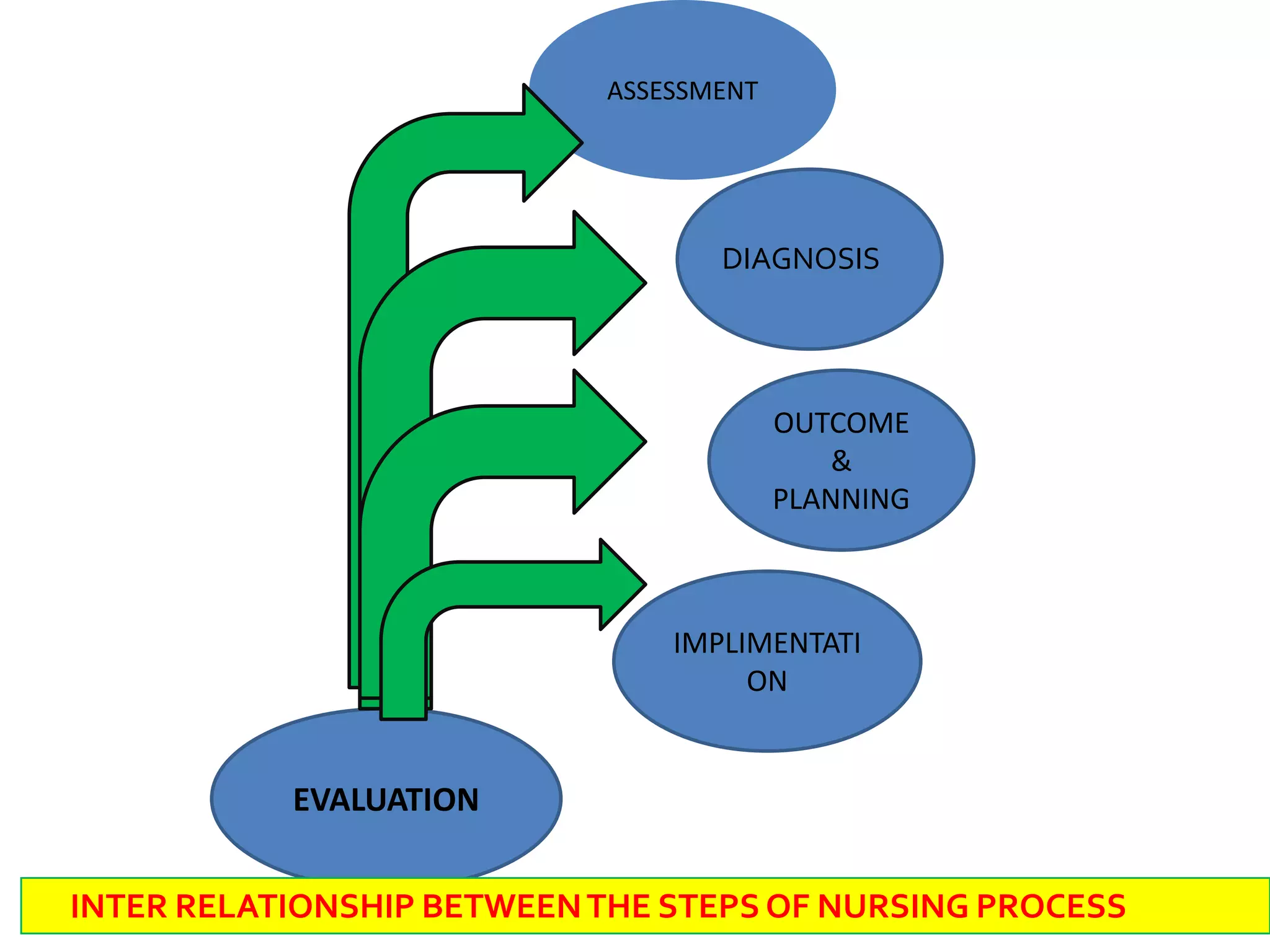
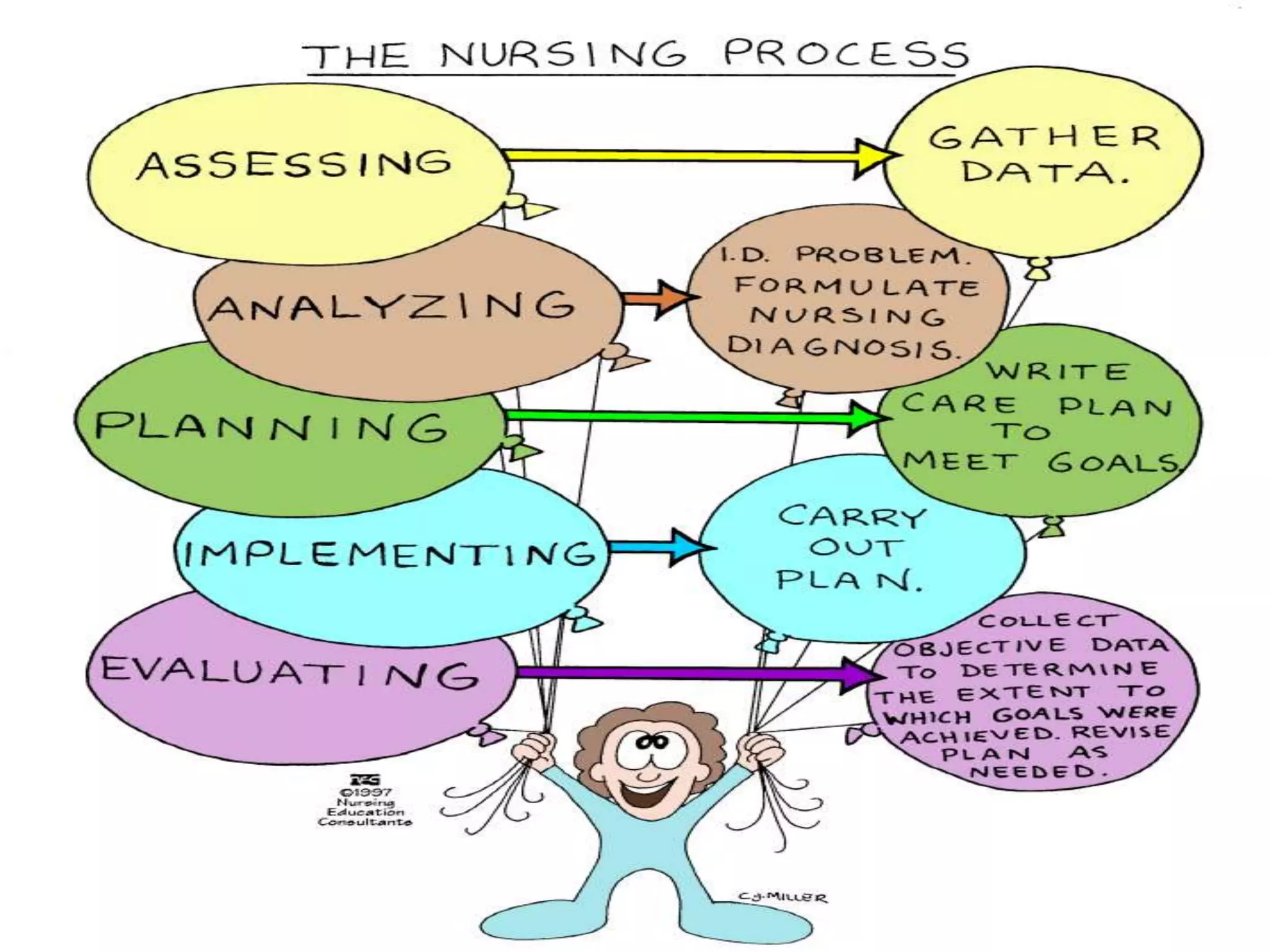
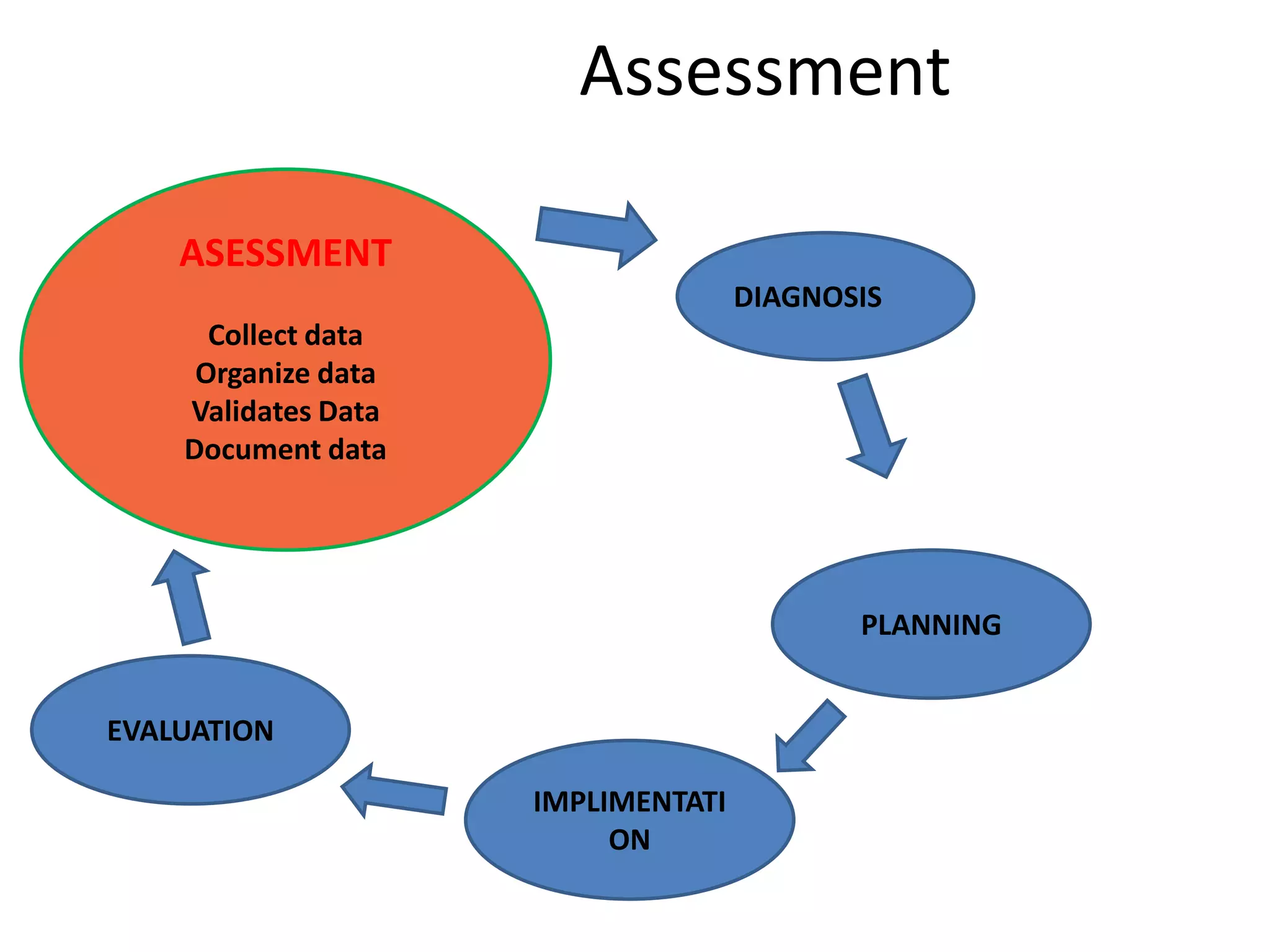
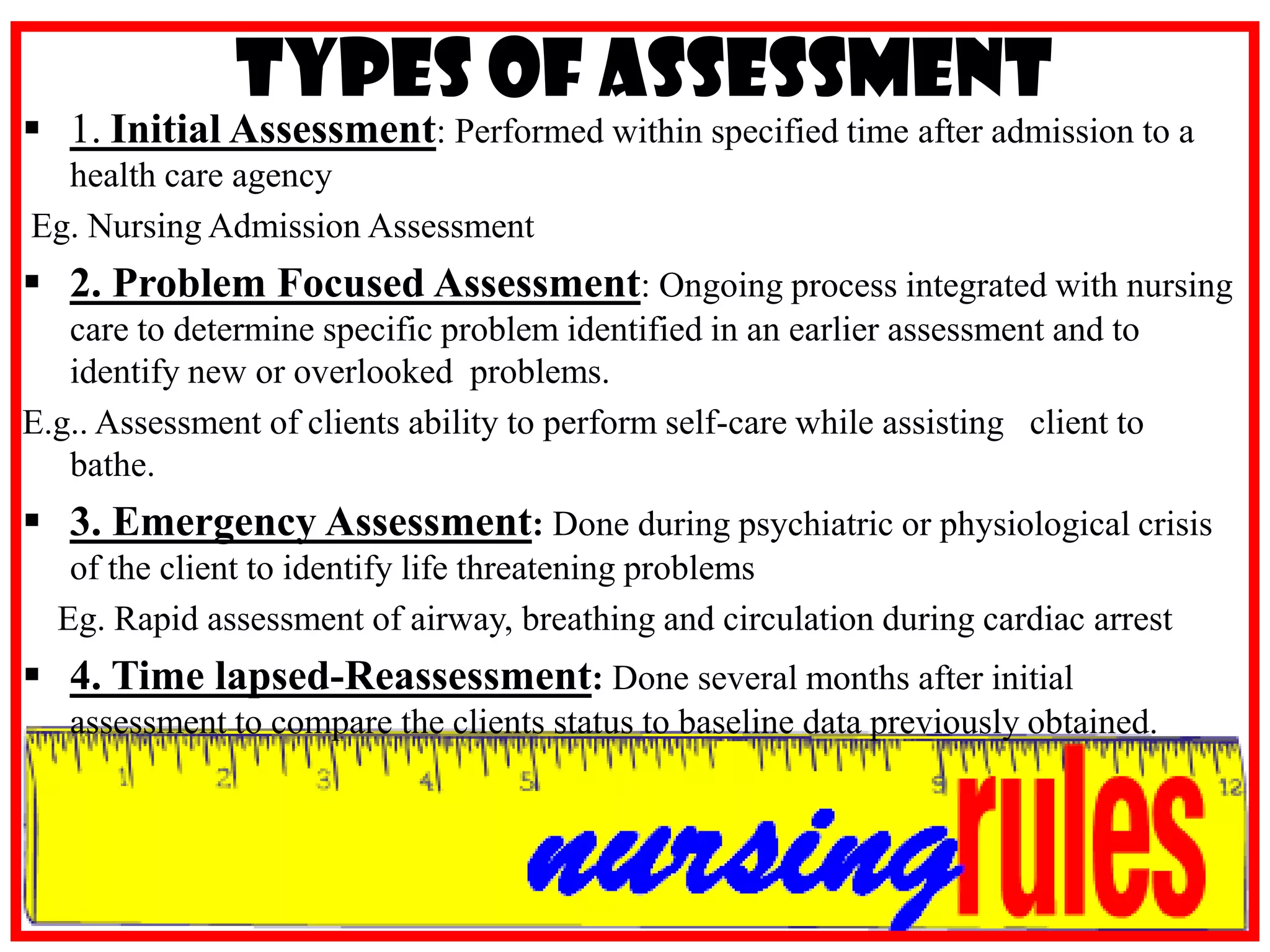
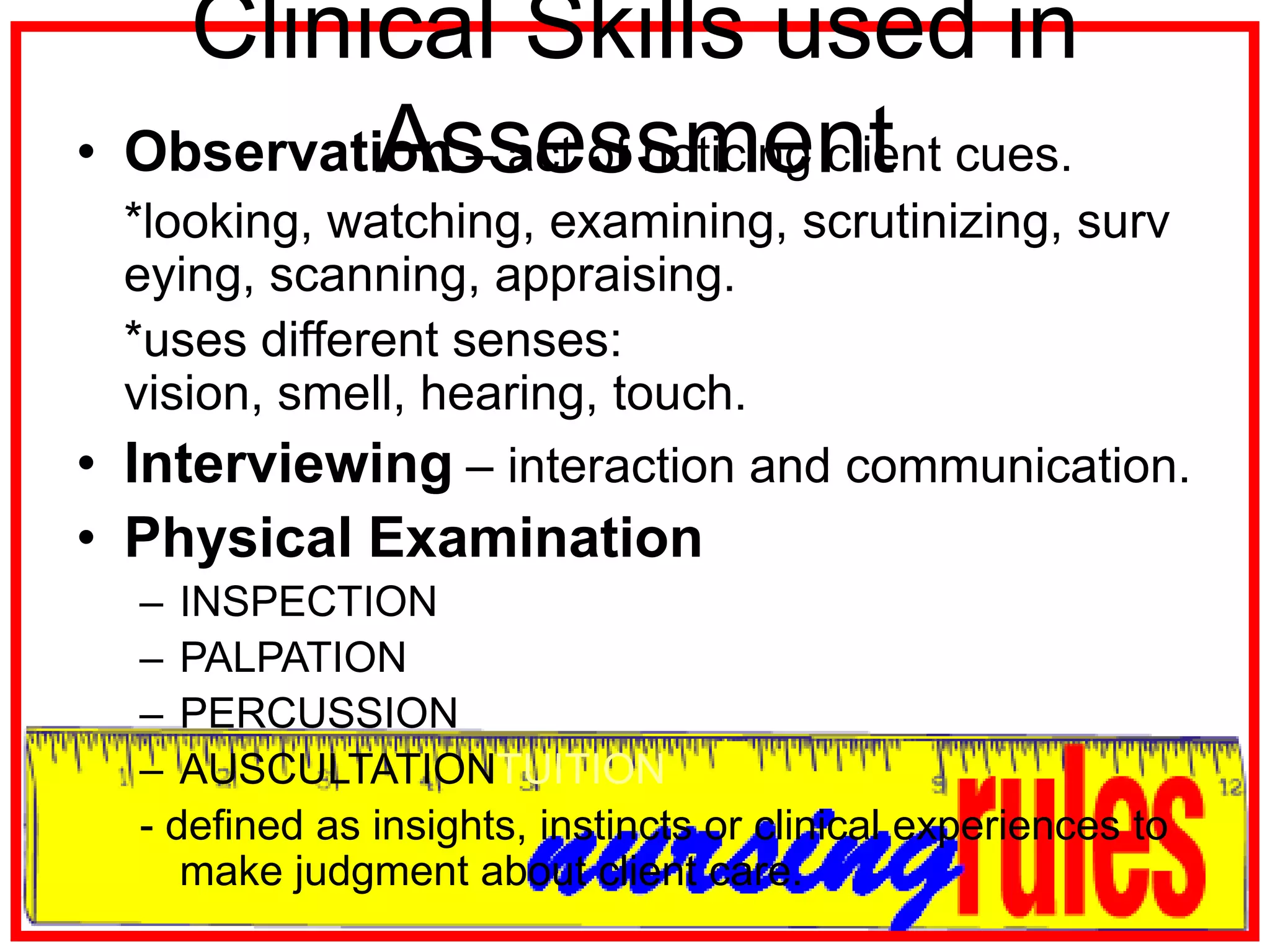
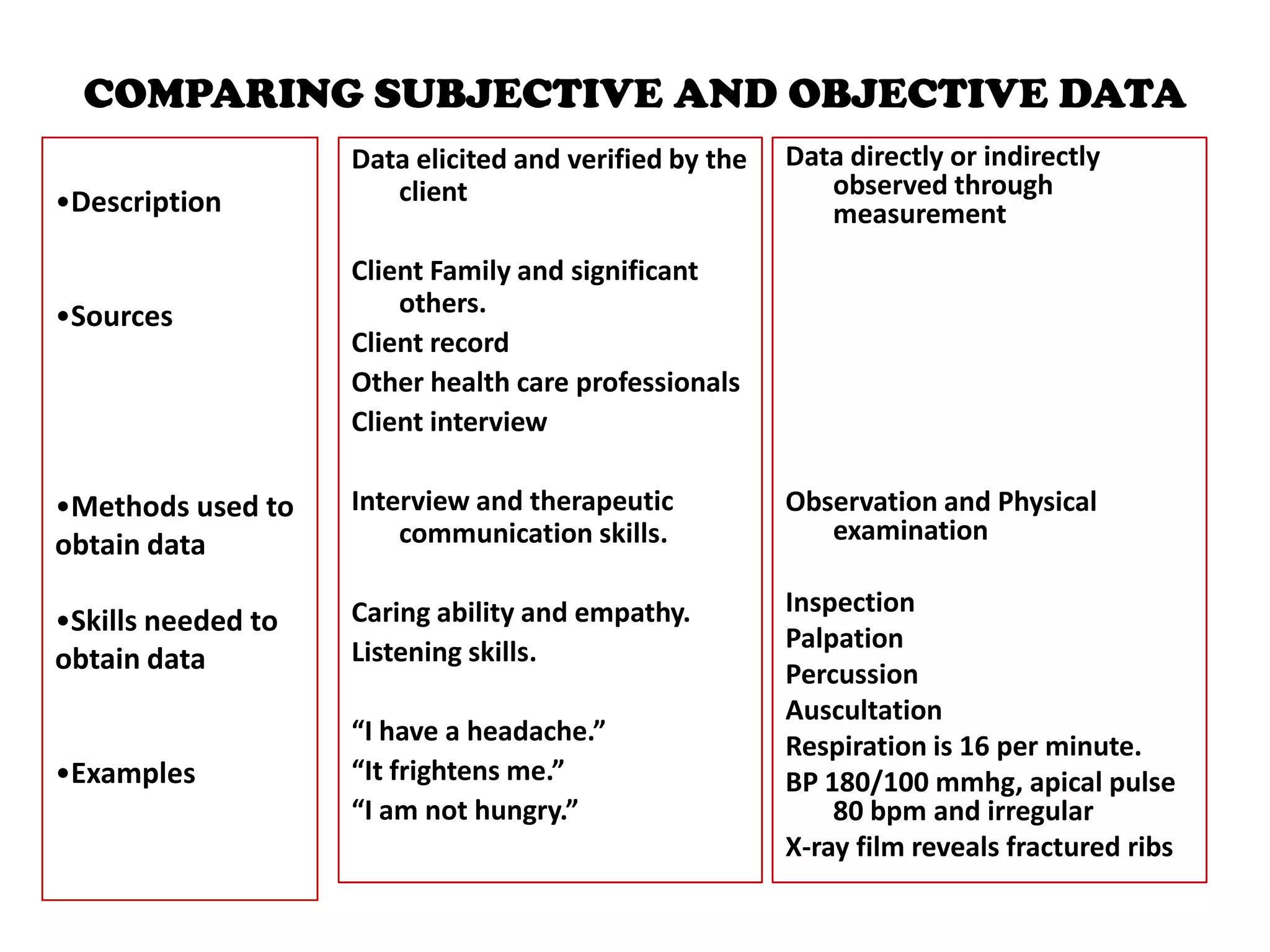
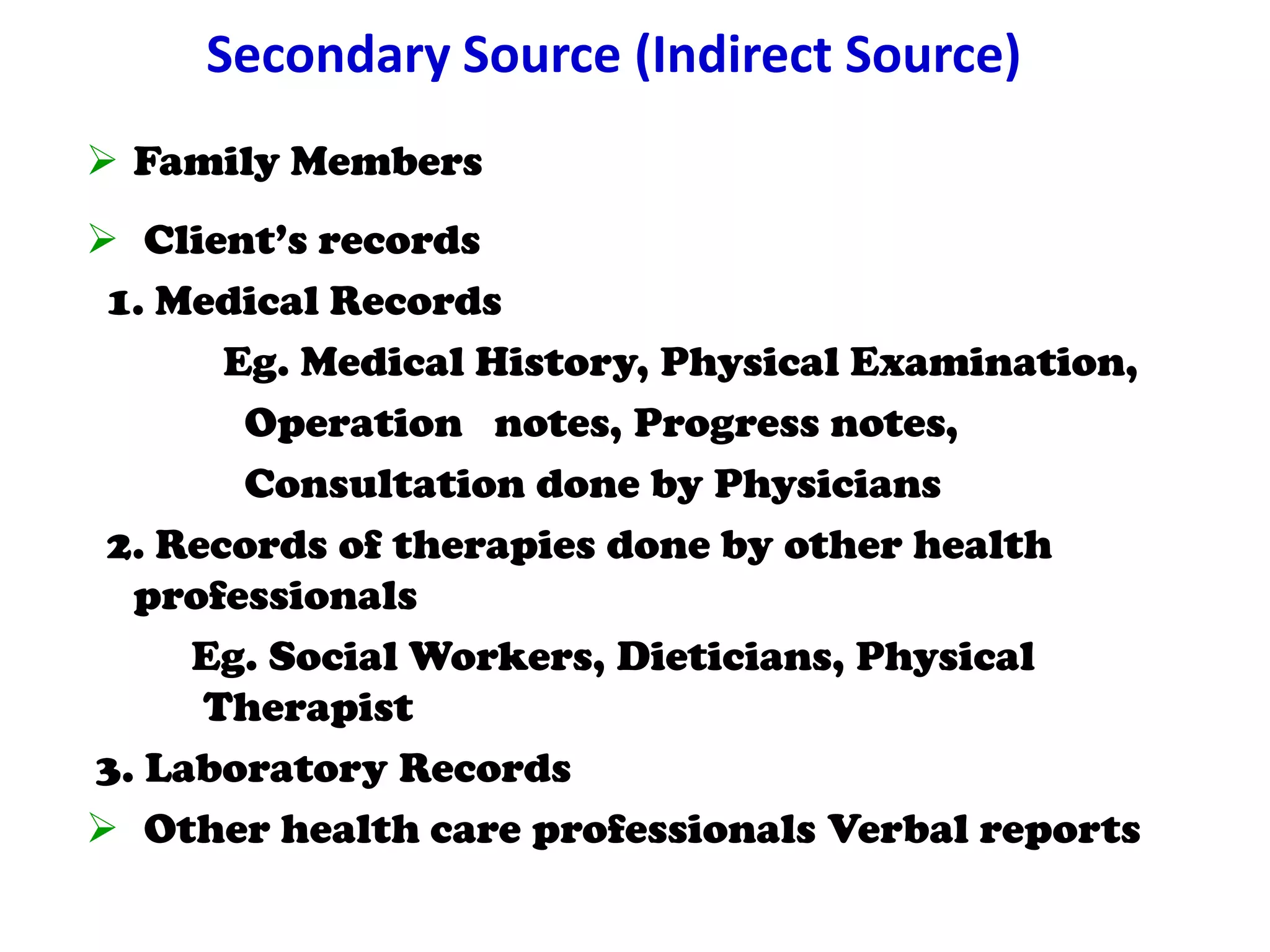
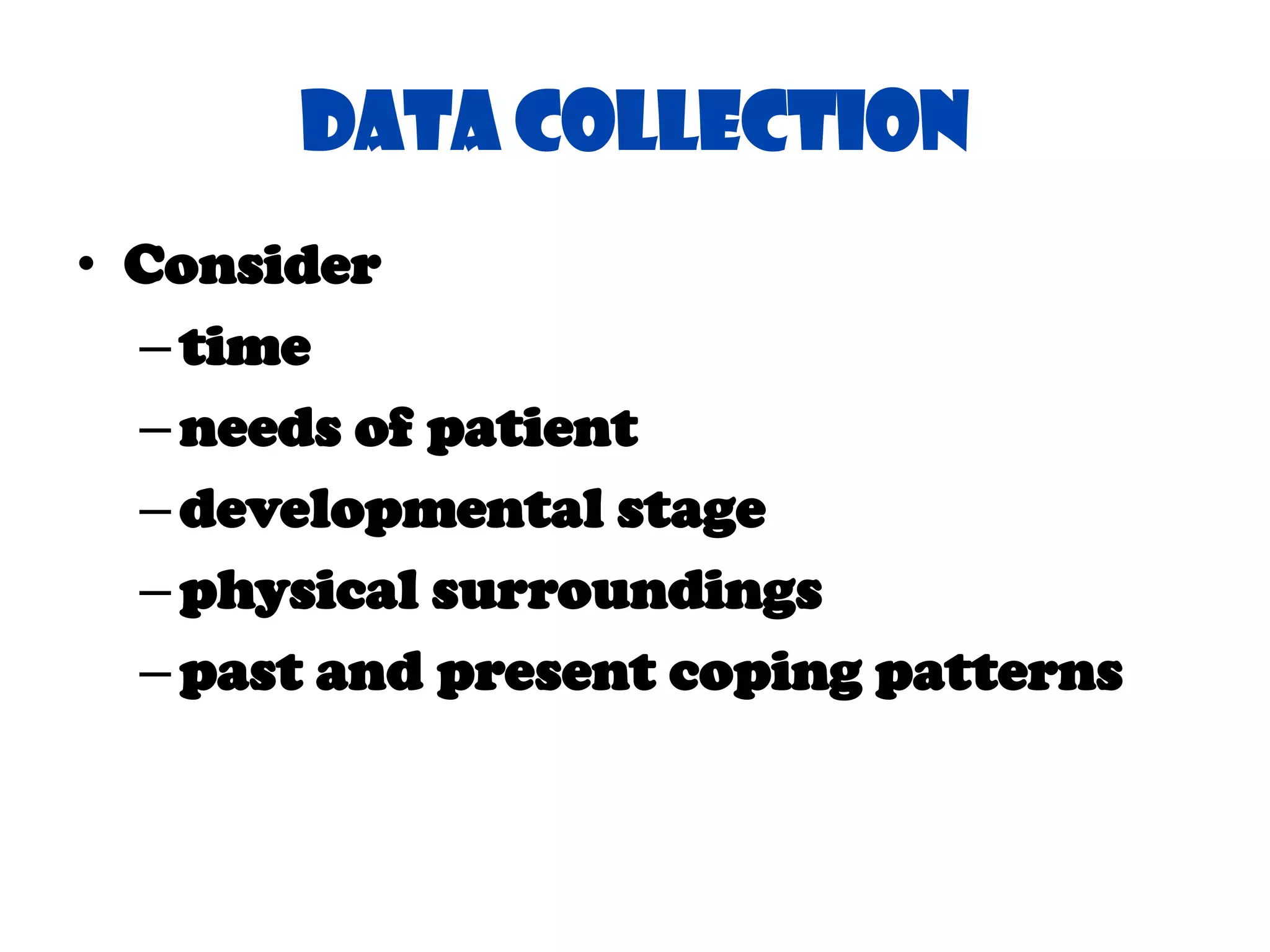
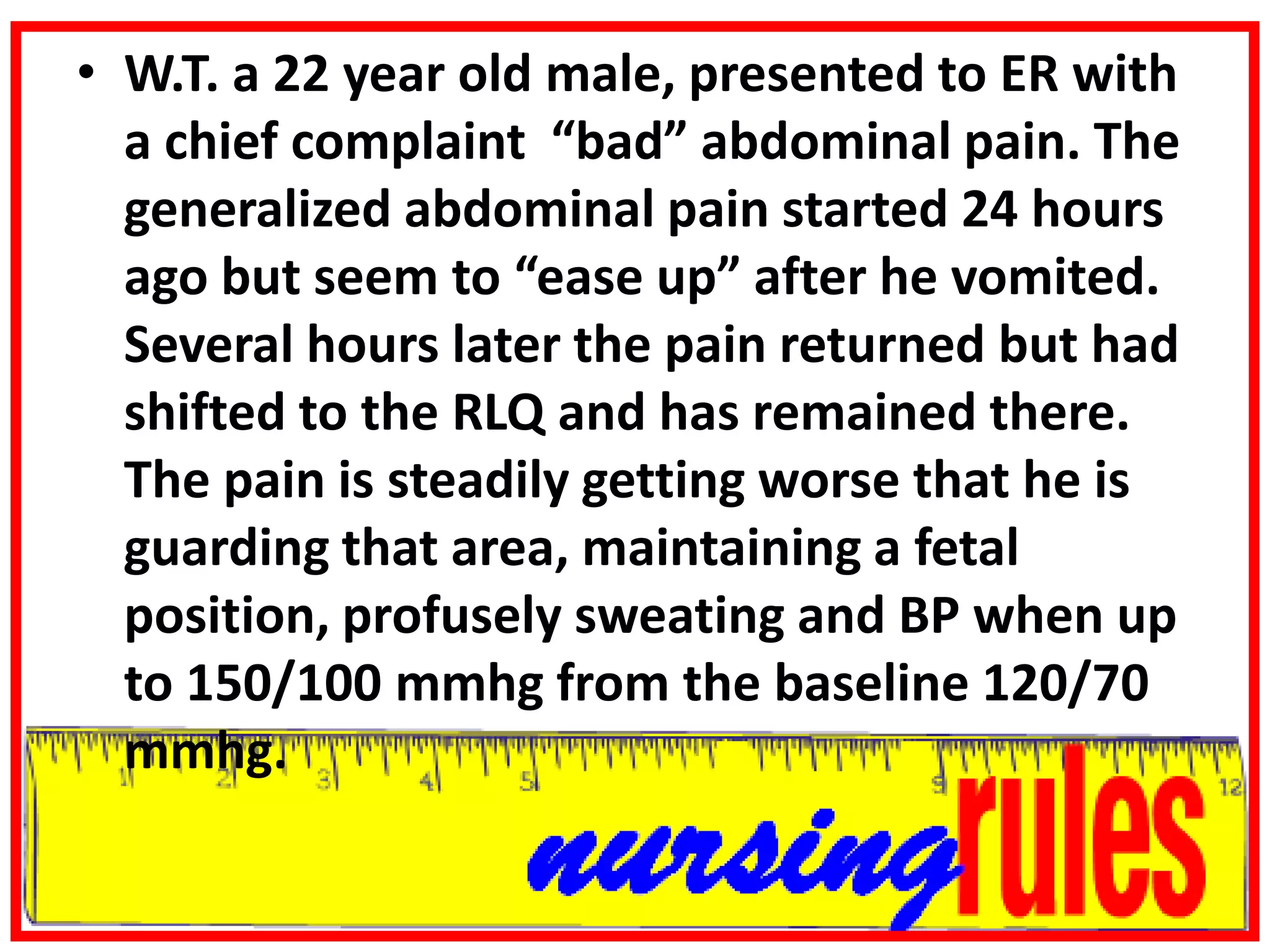
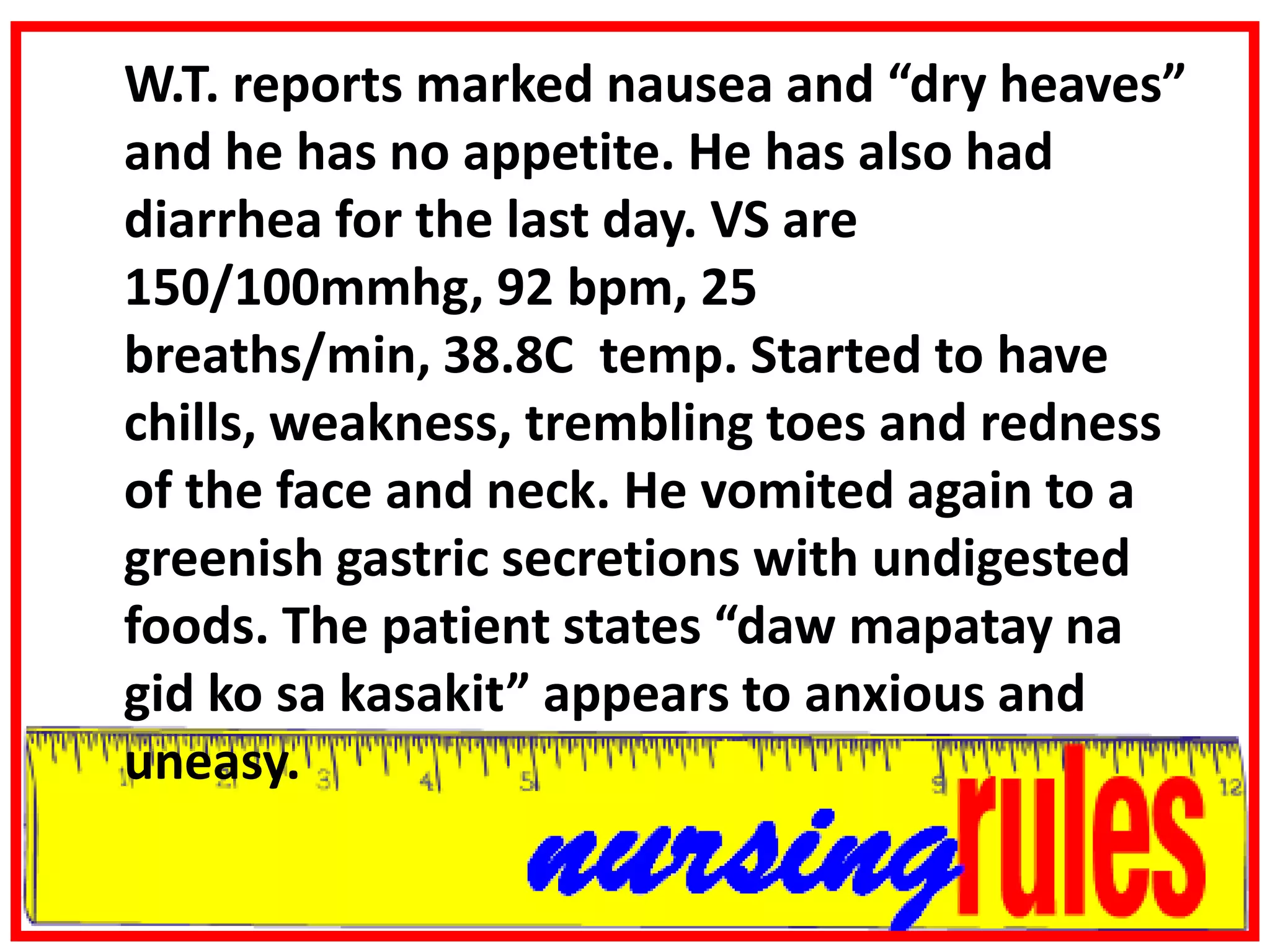
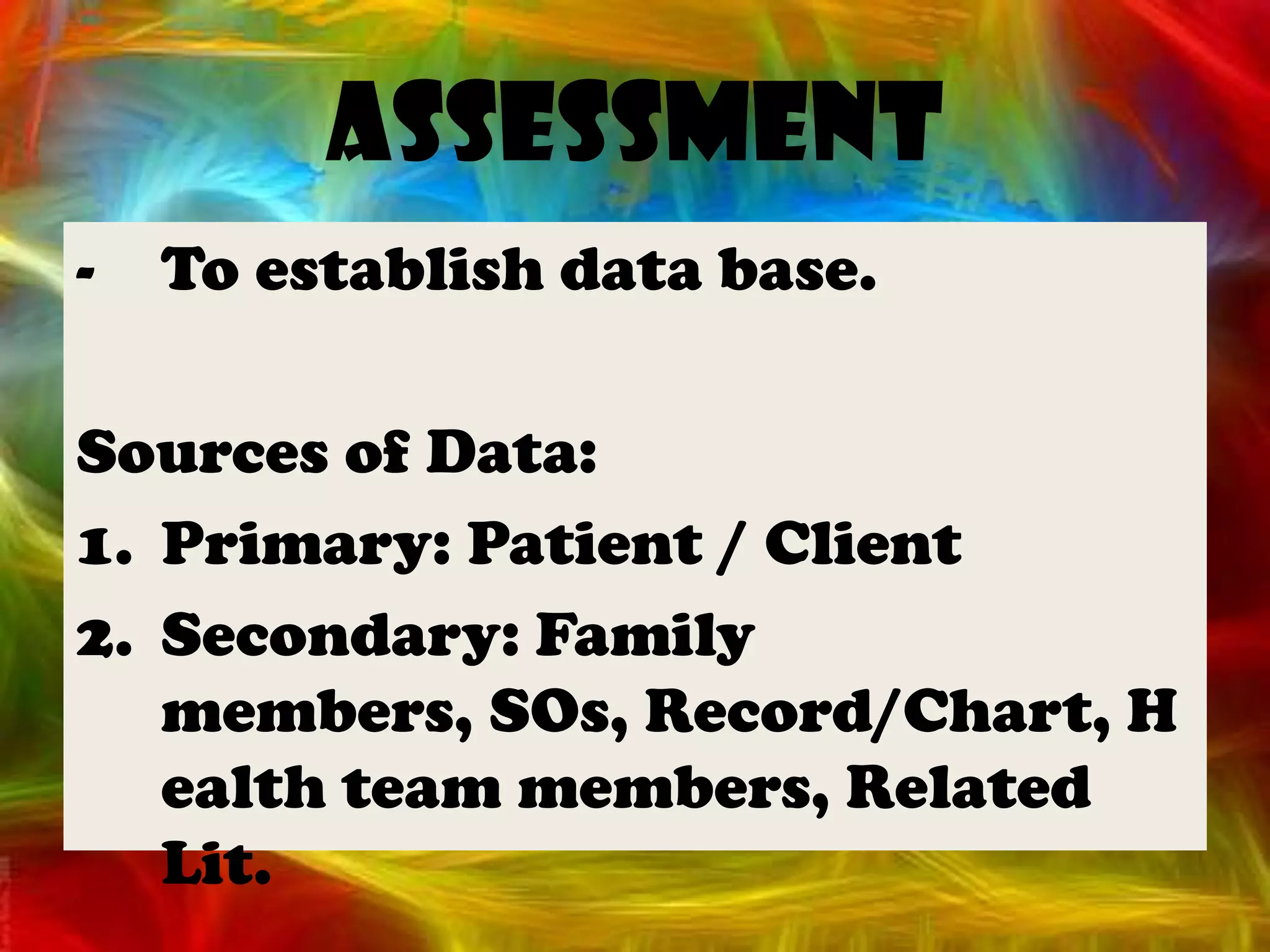
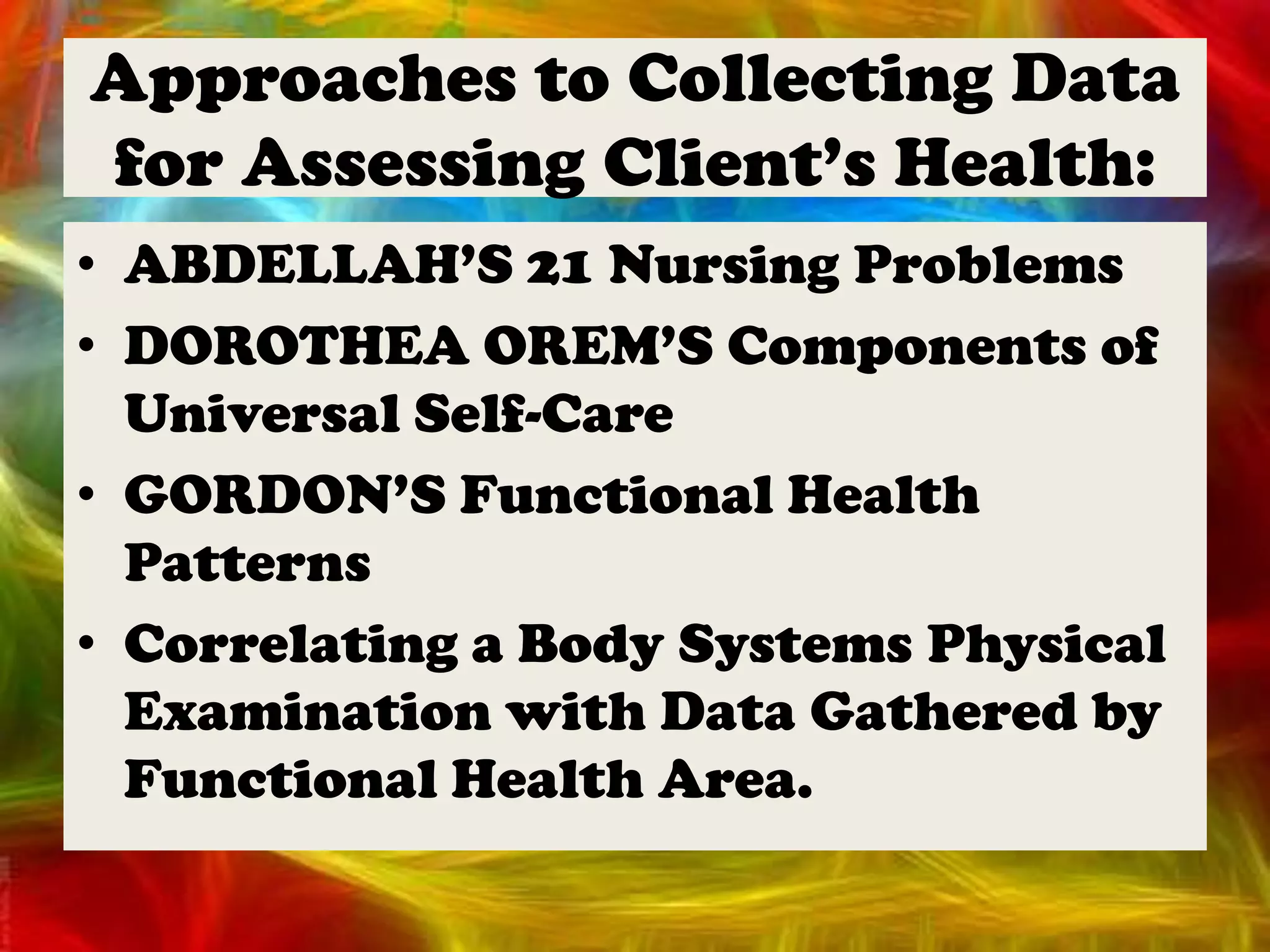
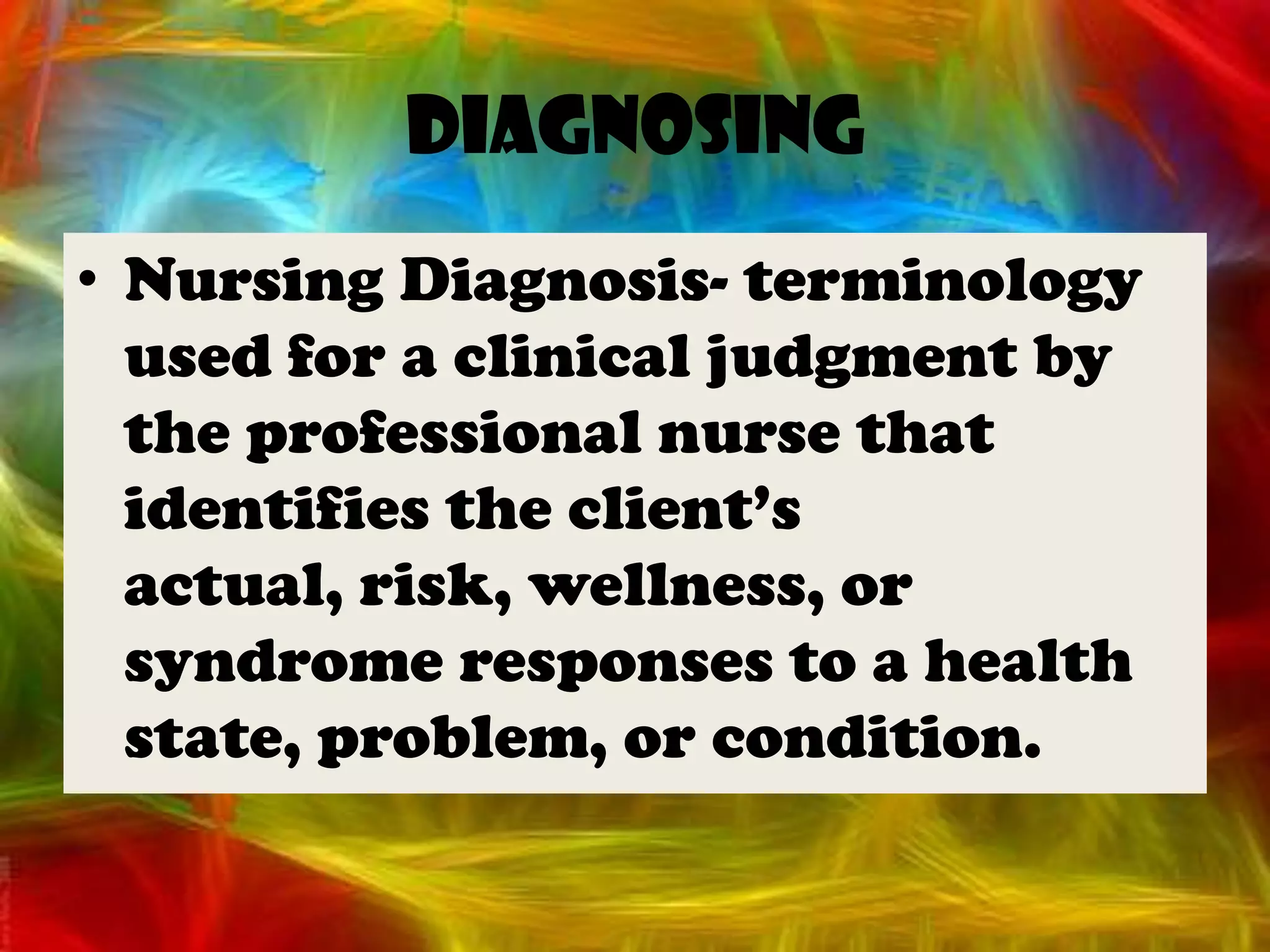
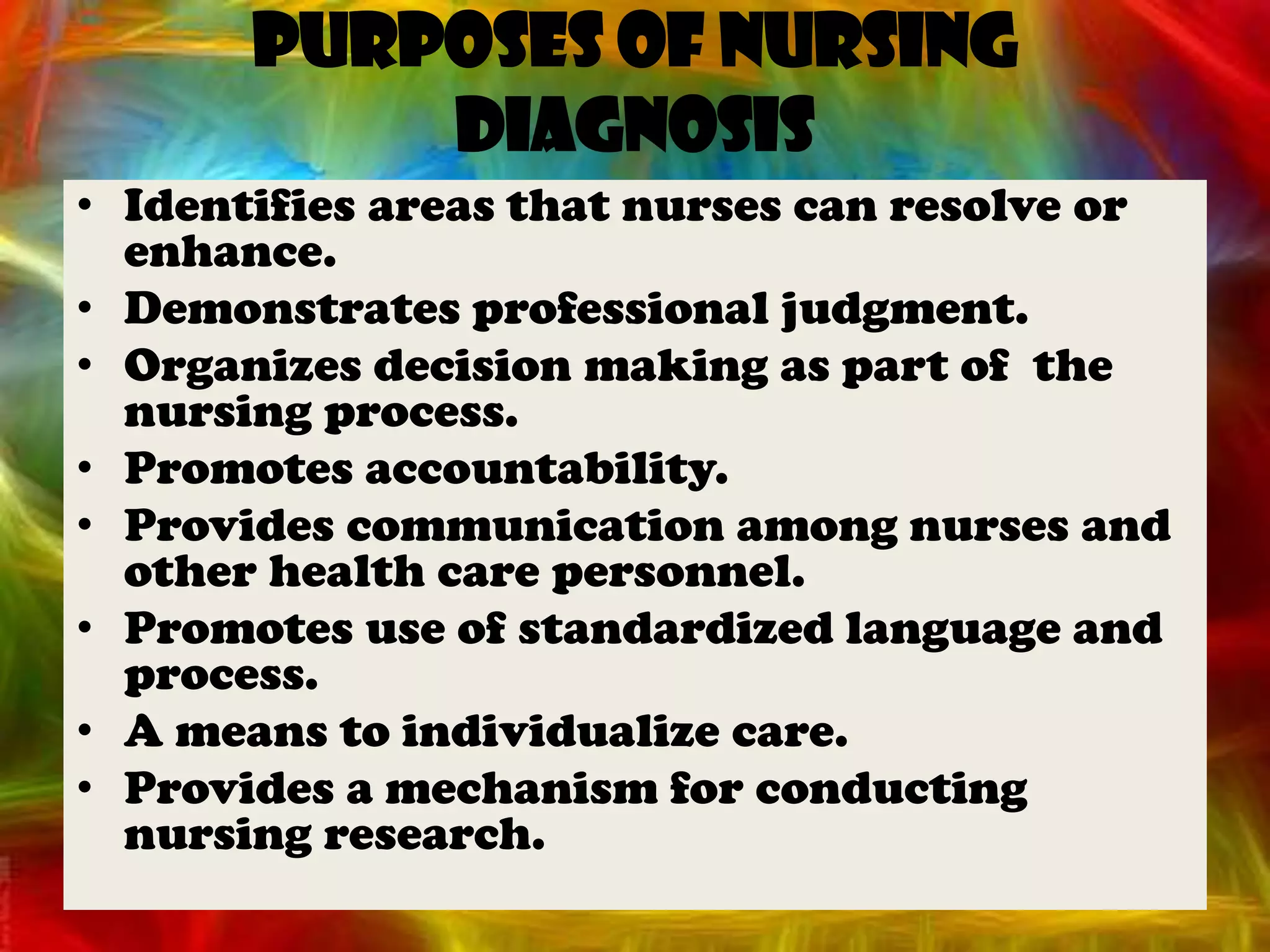
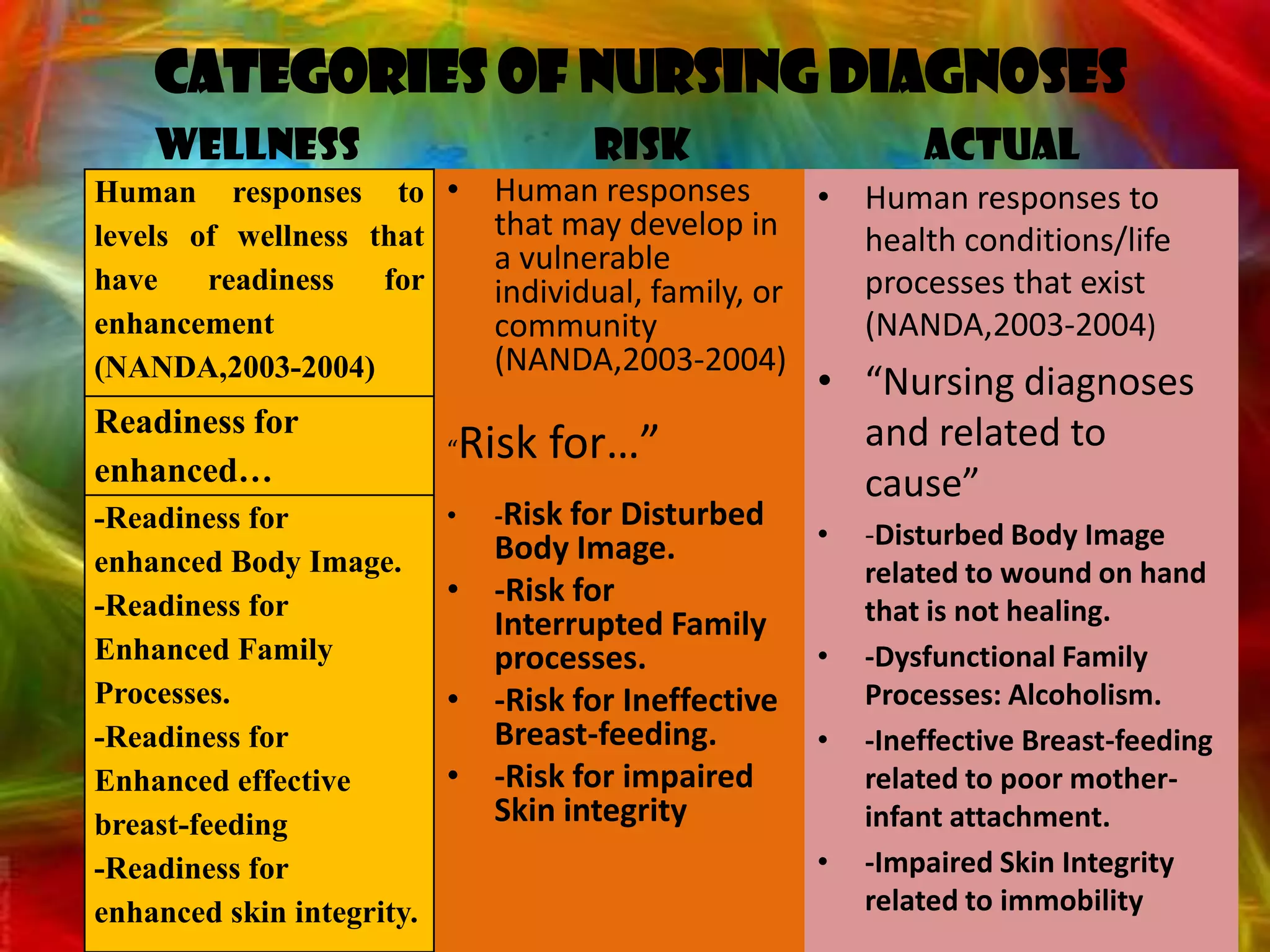
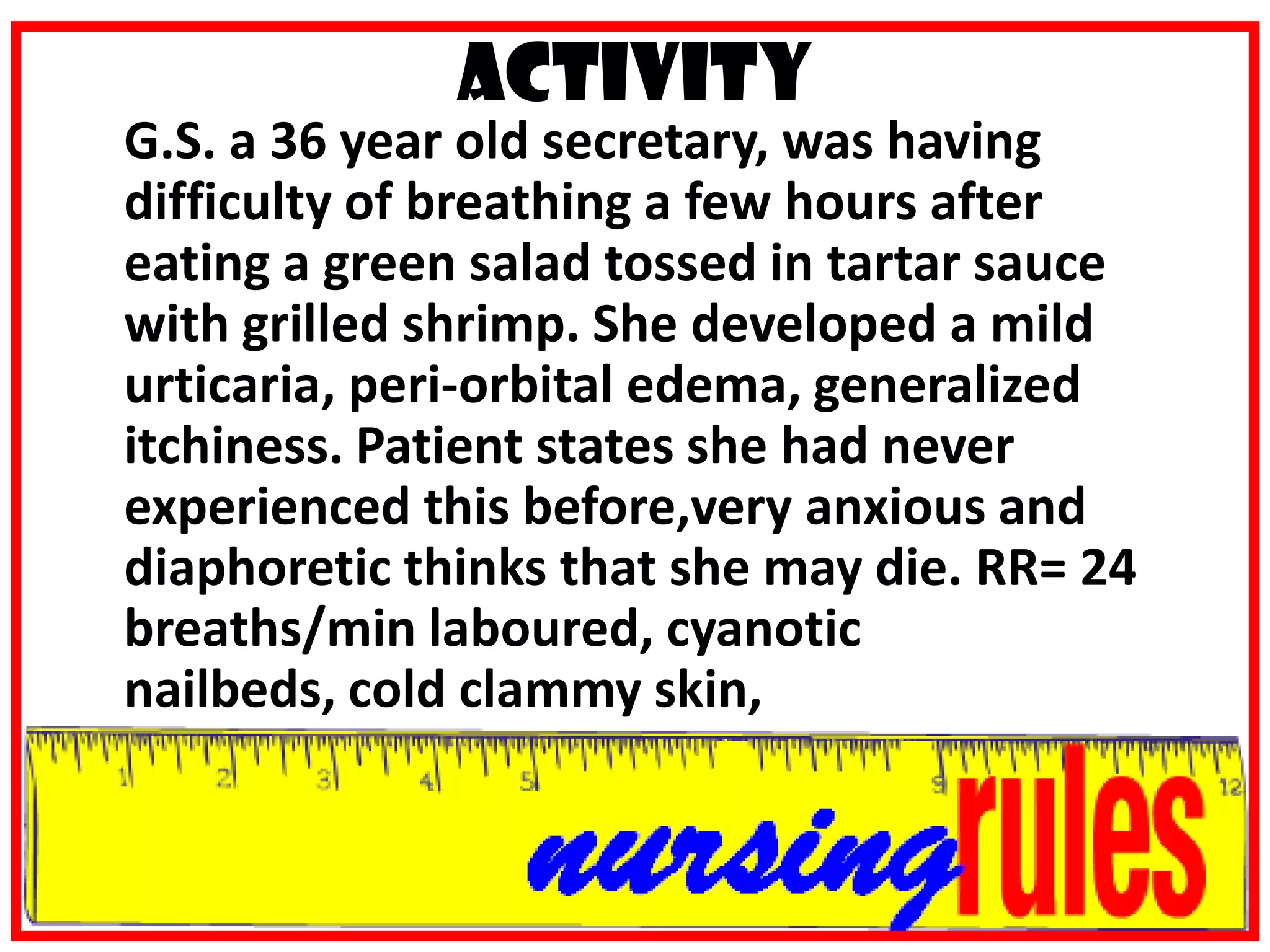
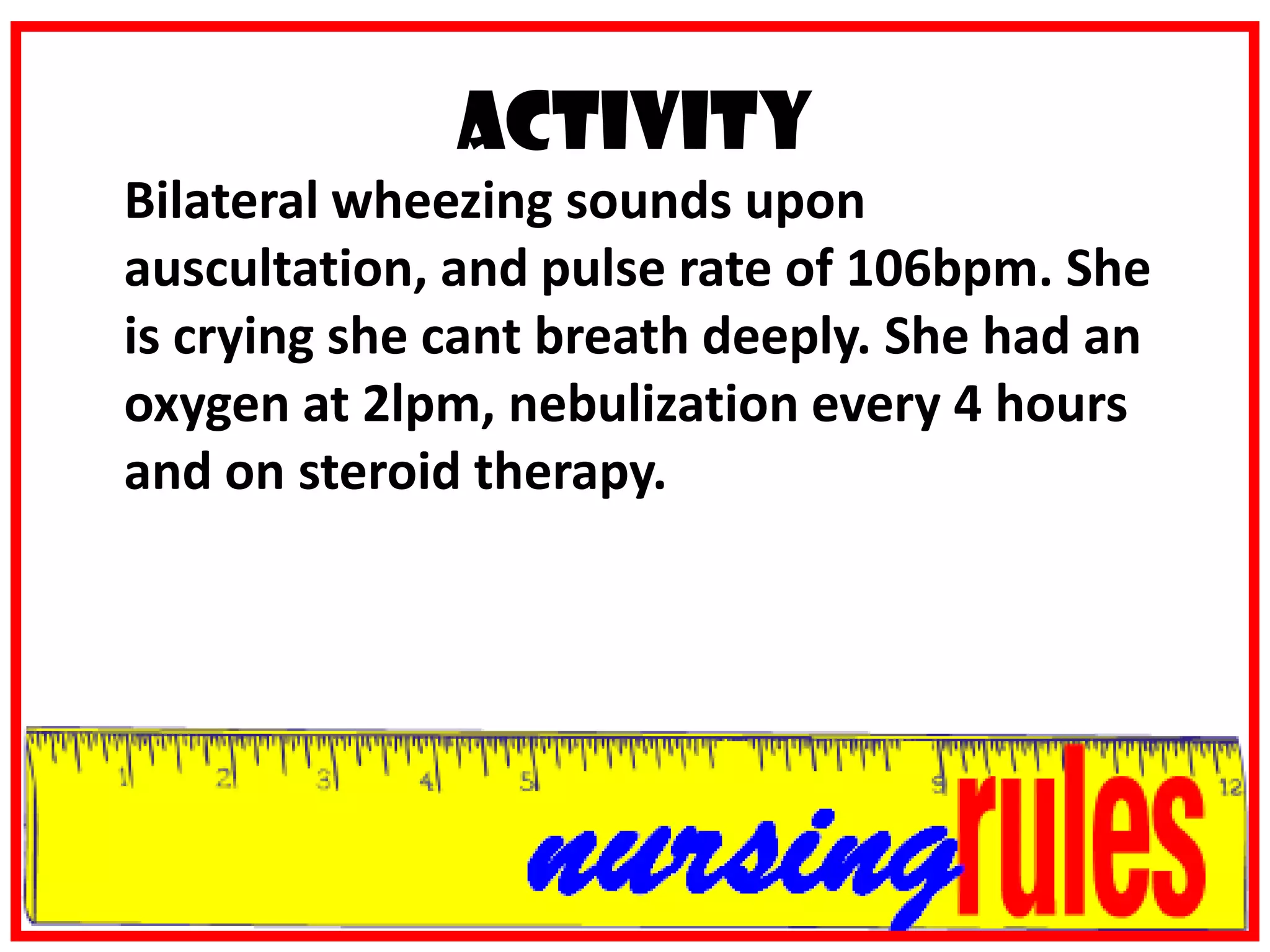
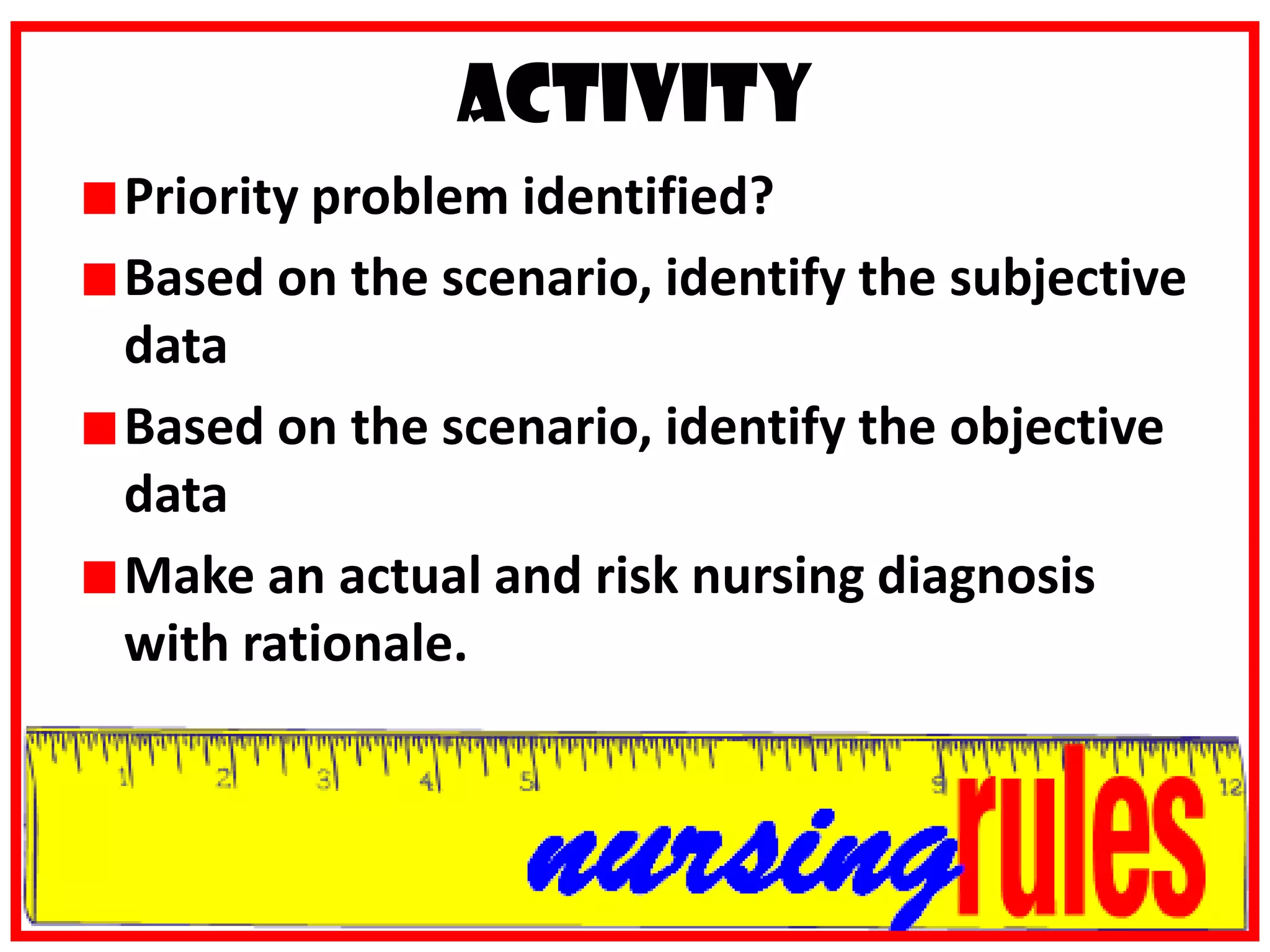
The course deals with concepts, principles and techniques of health assessment, including history taking, physical examination, psychosocial assessment and interpreting laboratory findings to determine nursing diagnoses across the lifespan. The course outline covers the nursing process, data collection, documentation, assessment techniques, vital signs, physical exams and diagnostic procedures. Students will learn to analyze health assessments, utilize the nursing process, demonstrate critical thinking and accurately collect, classify and document subjective and objective data.



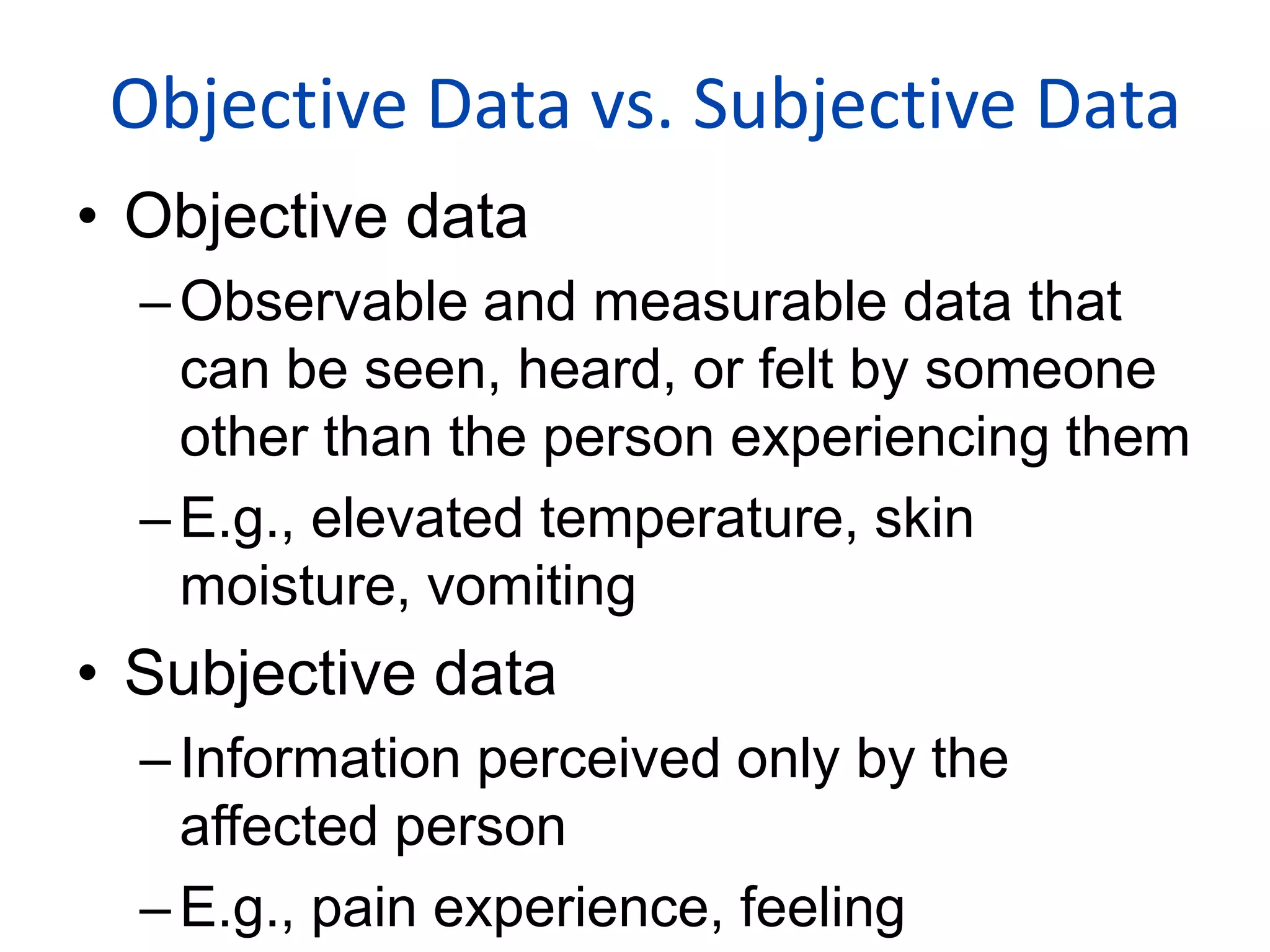








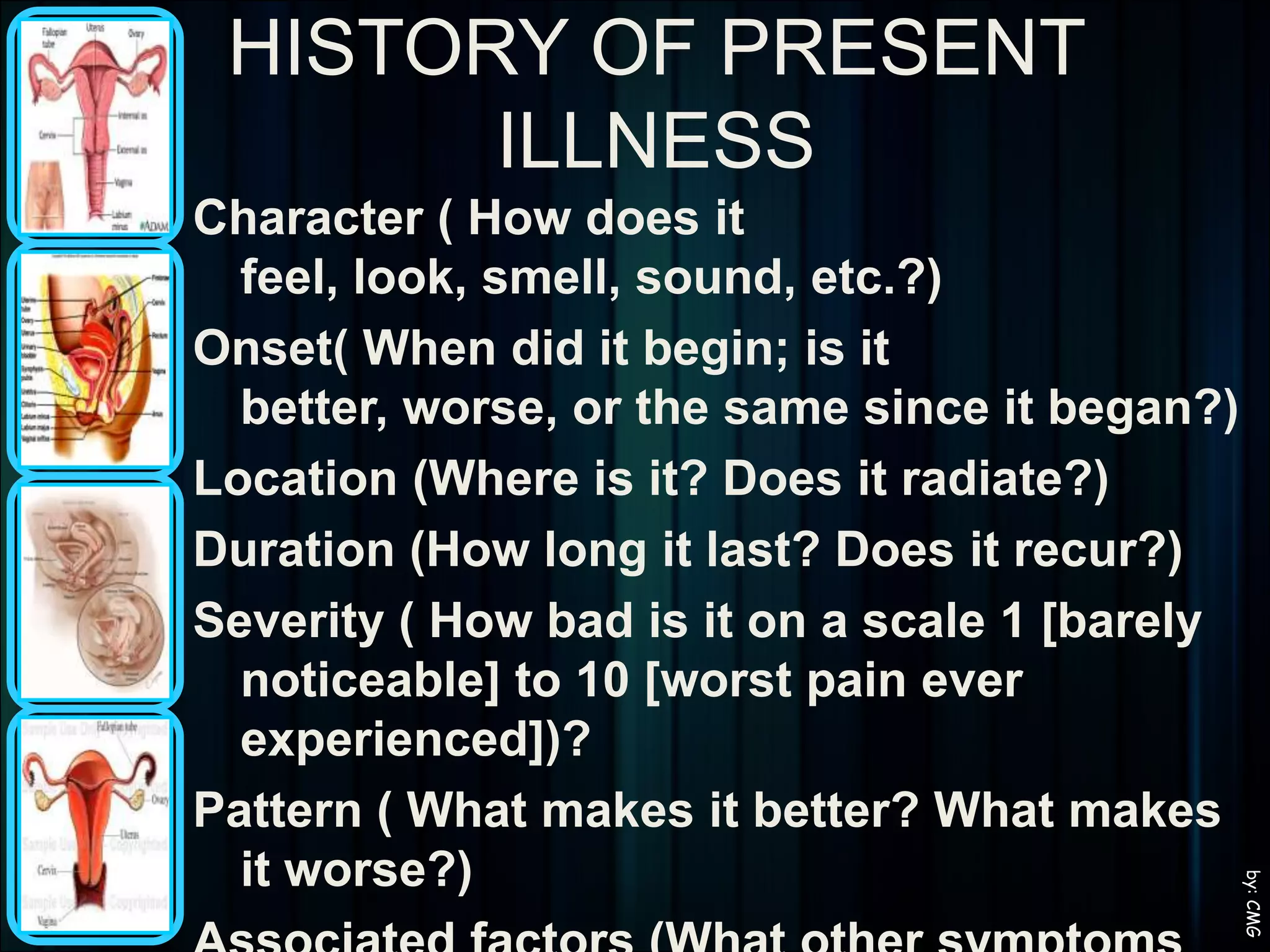



![HISTORY OF PRESENT ILLNESSCharacter ( How does it feel, look, smell, sound, etc.?)Onset( When did it begin; is it better, worse, or the same since it began?)Location (Where is it? Does it radiate?)Duration (How long it last? Does it recur?)Severity ( How bad is it on a scale 1 [barely noticeable] to 10 [worst pain ever experienced])?Pattern ( What makes it better? What makes it worse?)Associated factors (What other symptoms do you have with it? Will you be able to continue doing your work or other activities? by: CMG](https://image.slidesharecdn.com/nursingprocess-100221043419-phpapp02/75/Nursing-Process-160-2048.jpg)