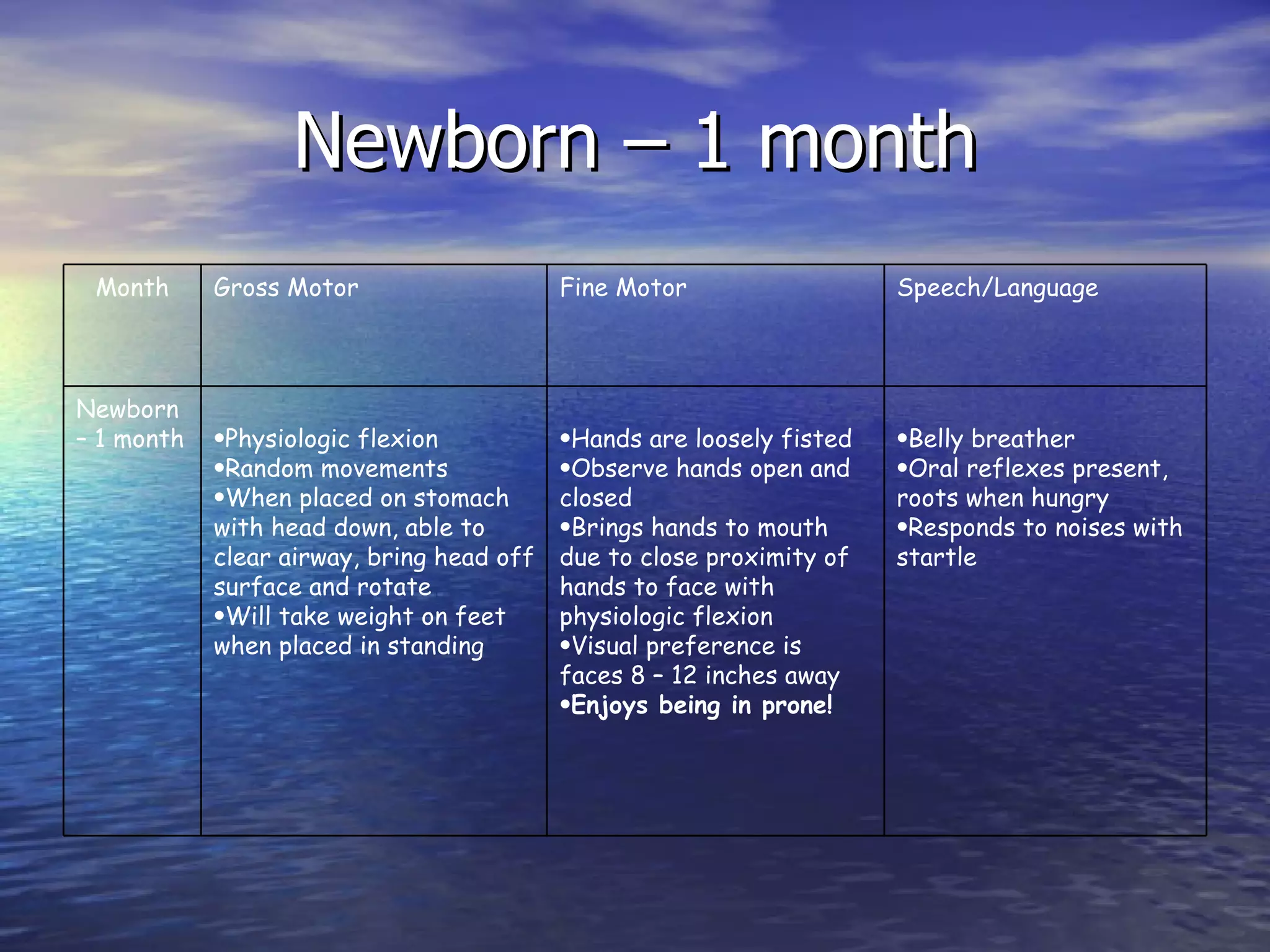
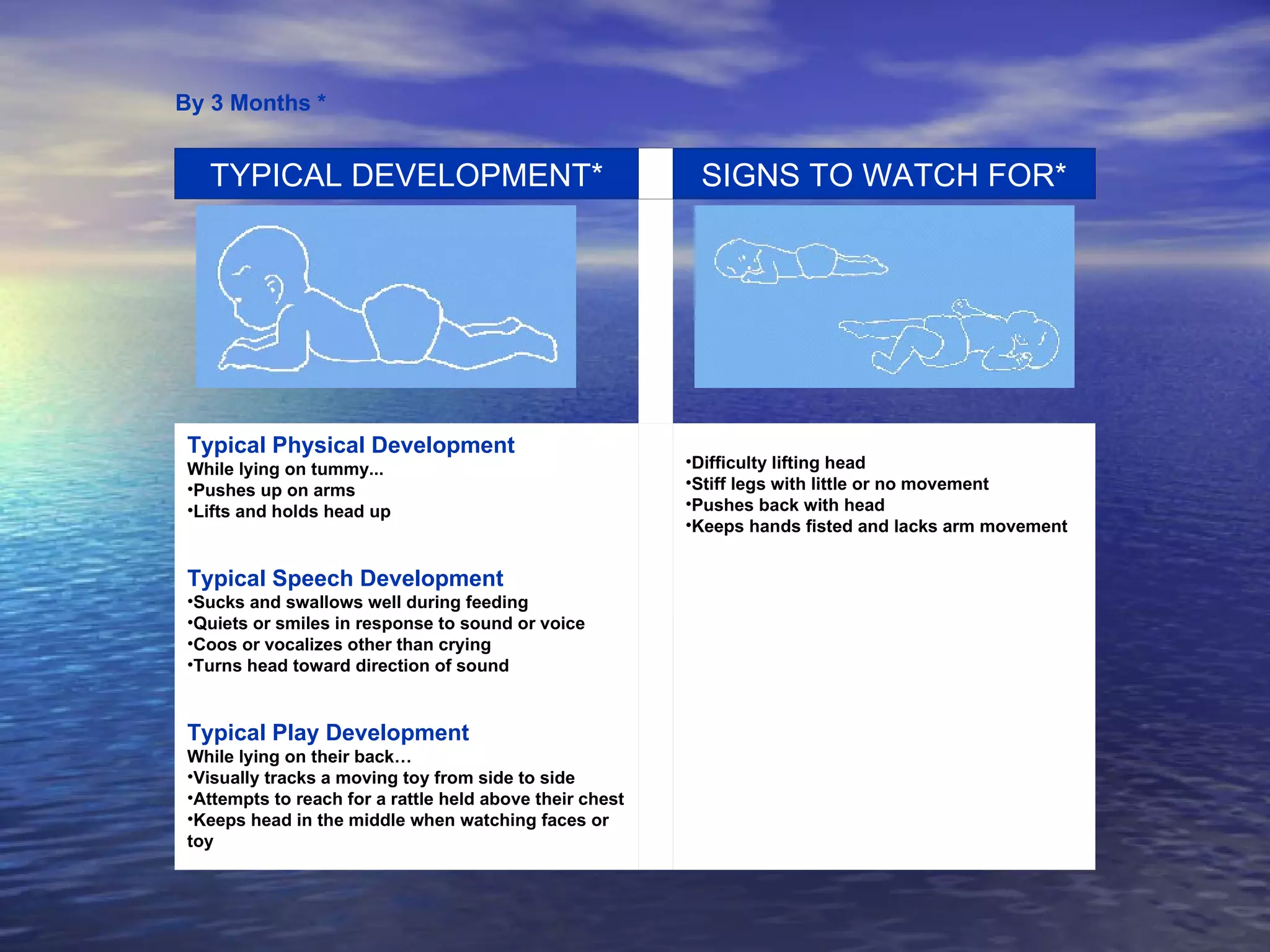
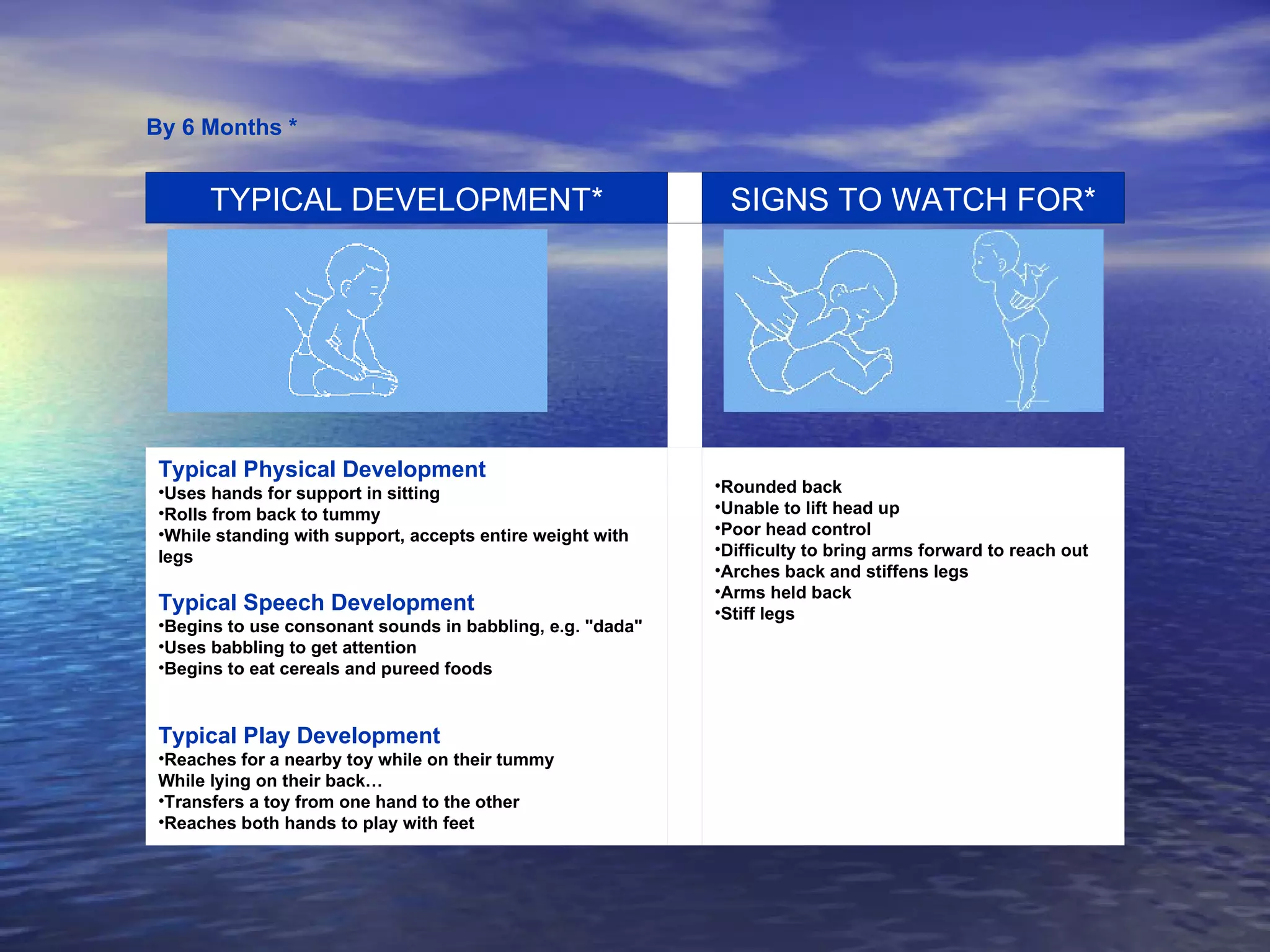
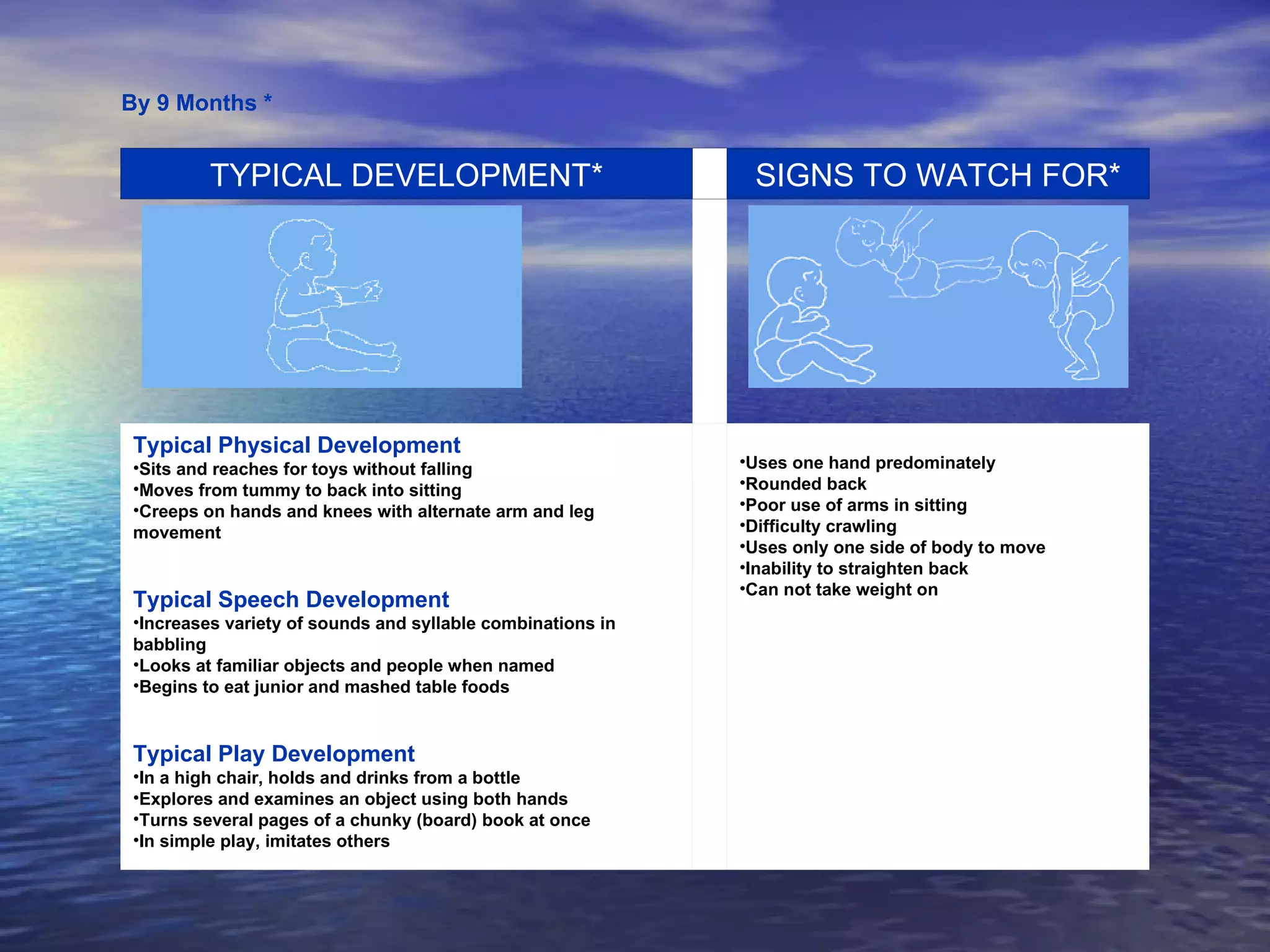
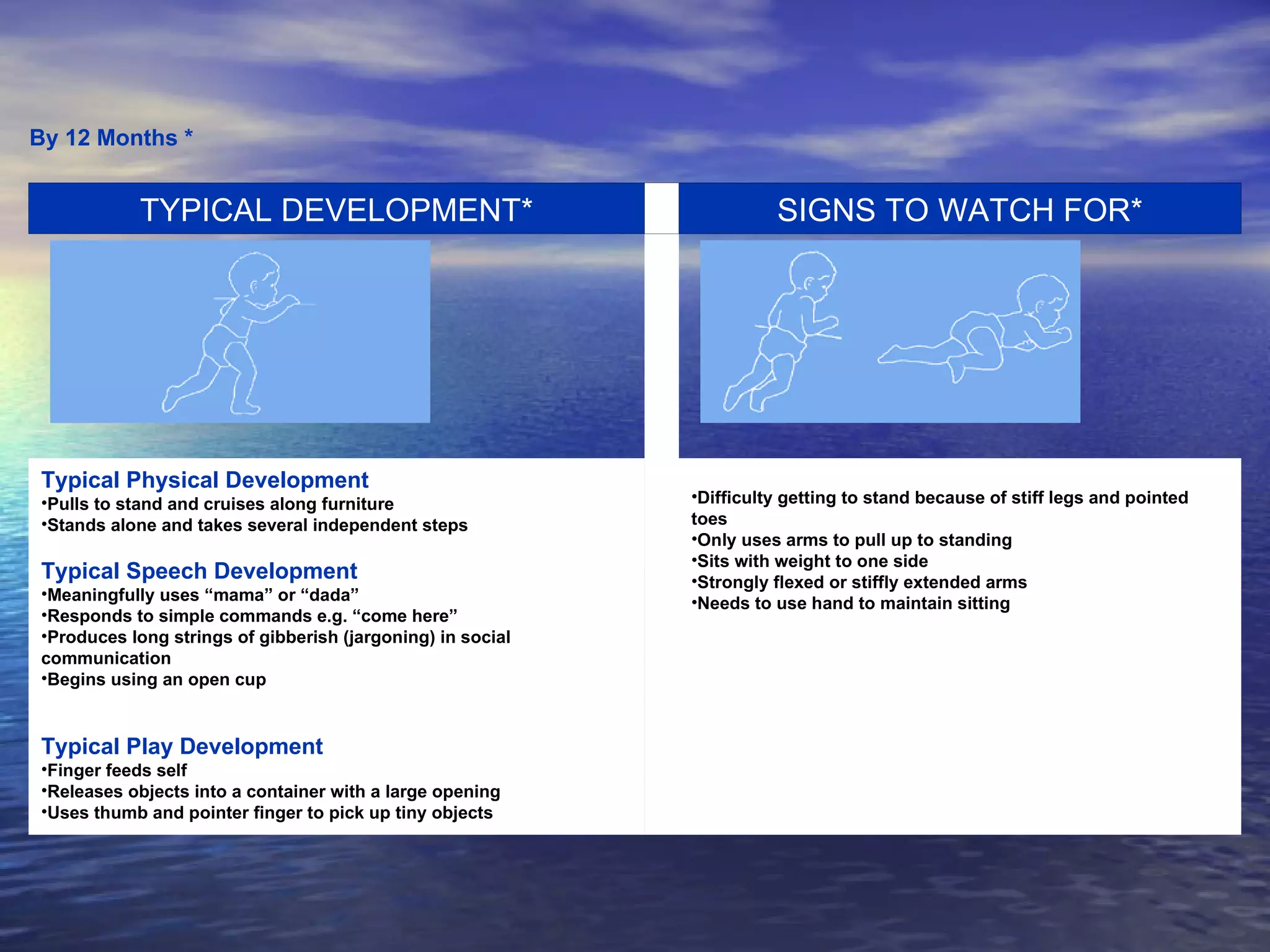
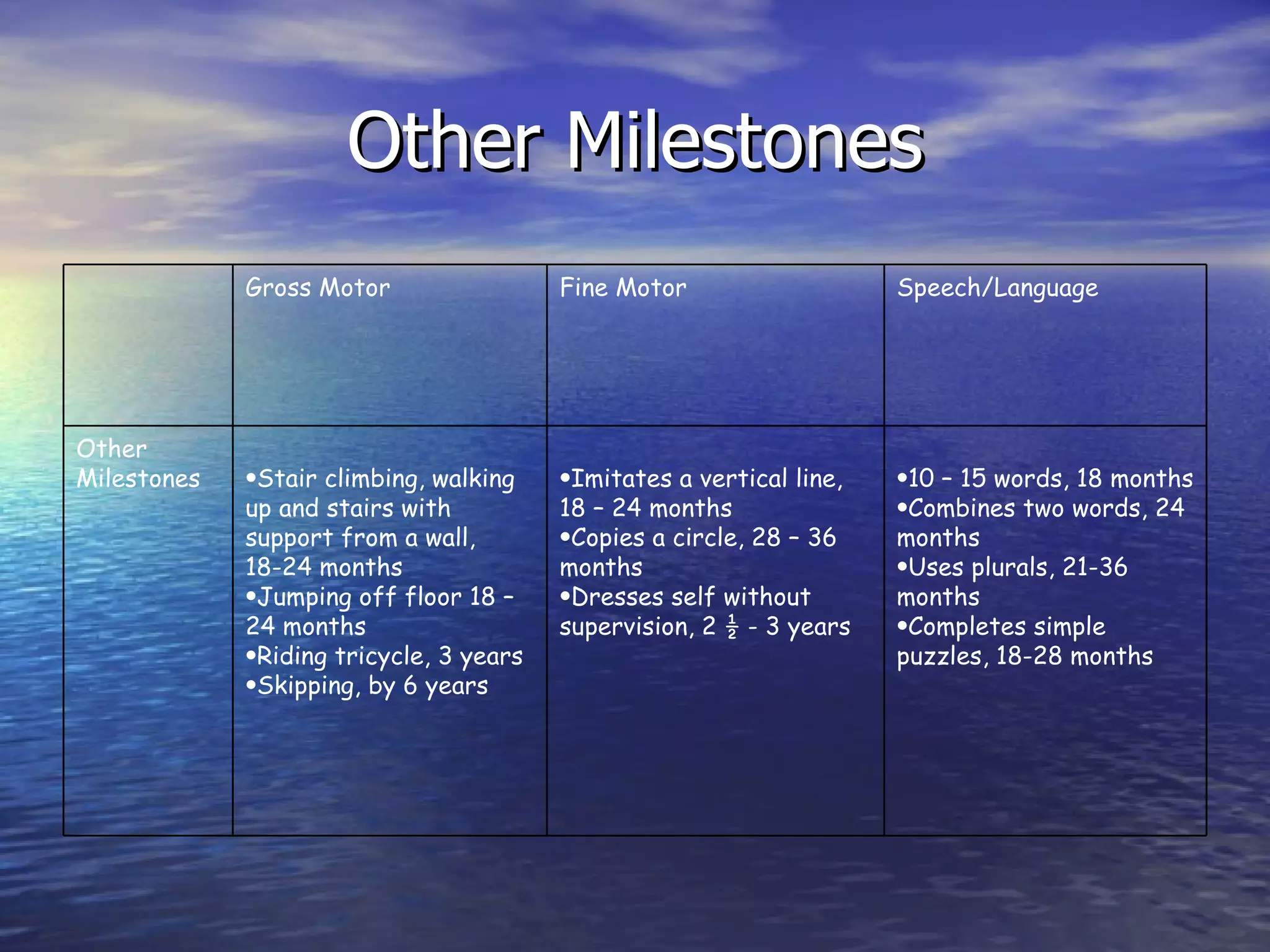
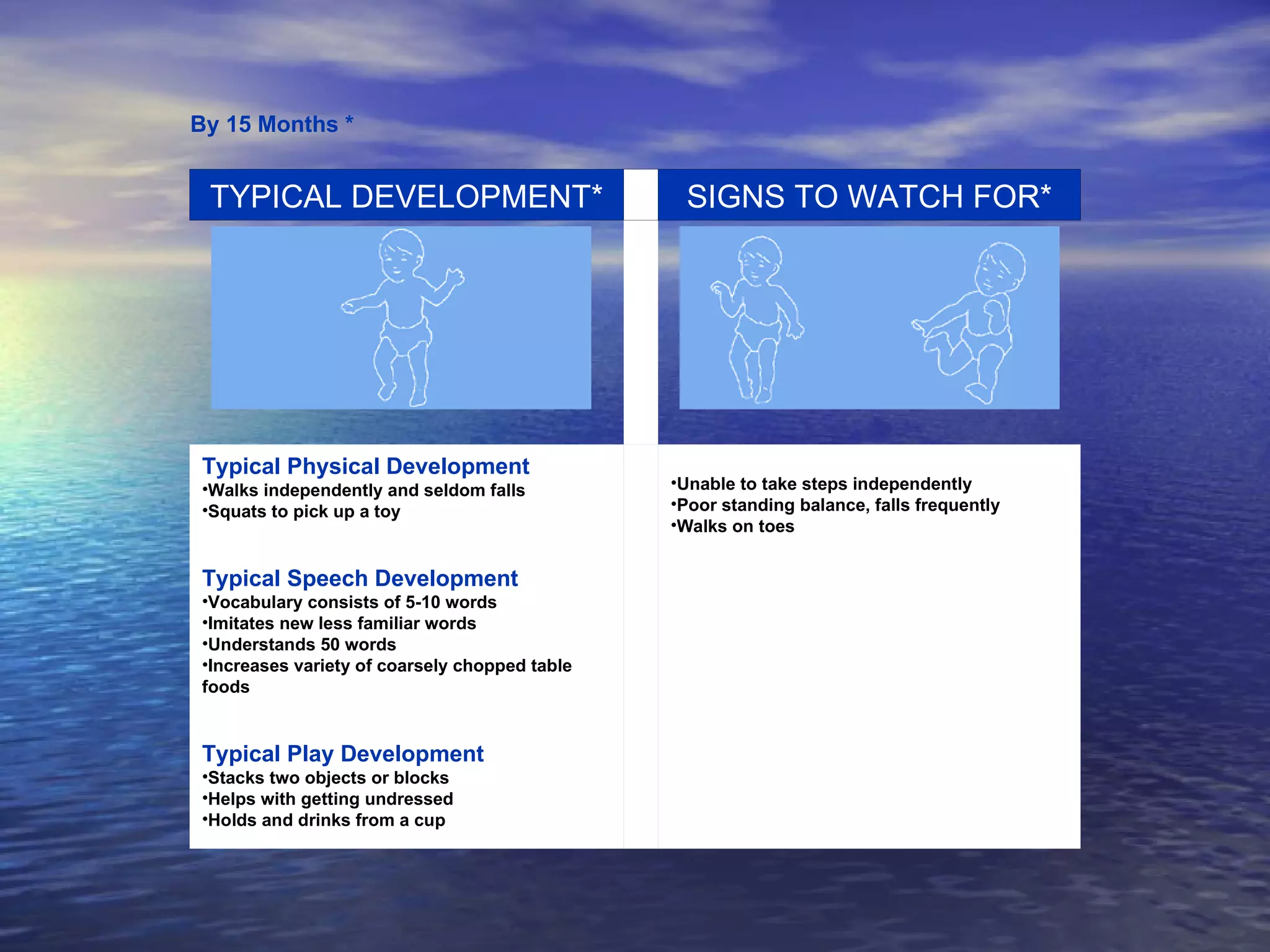
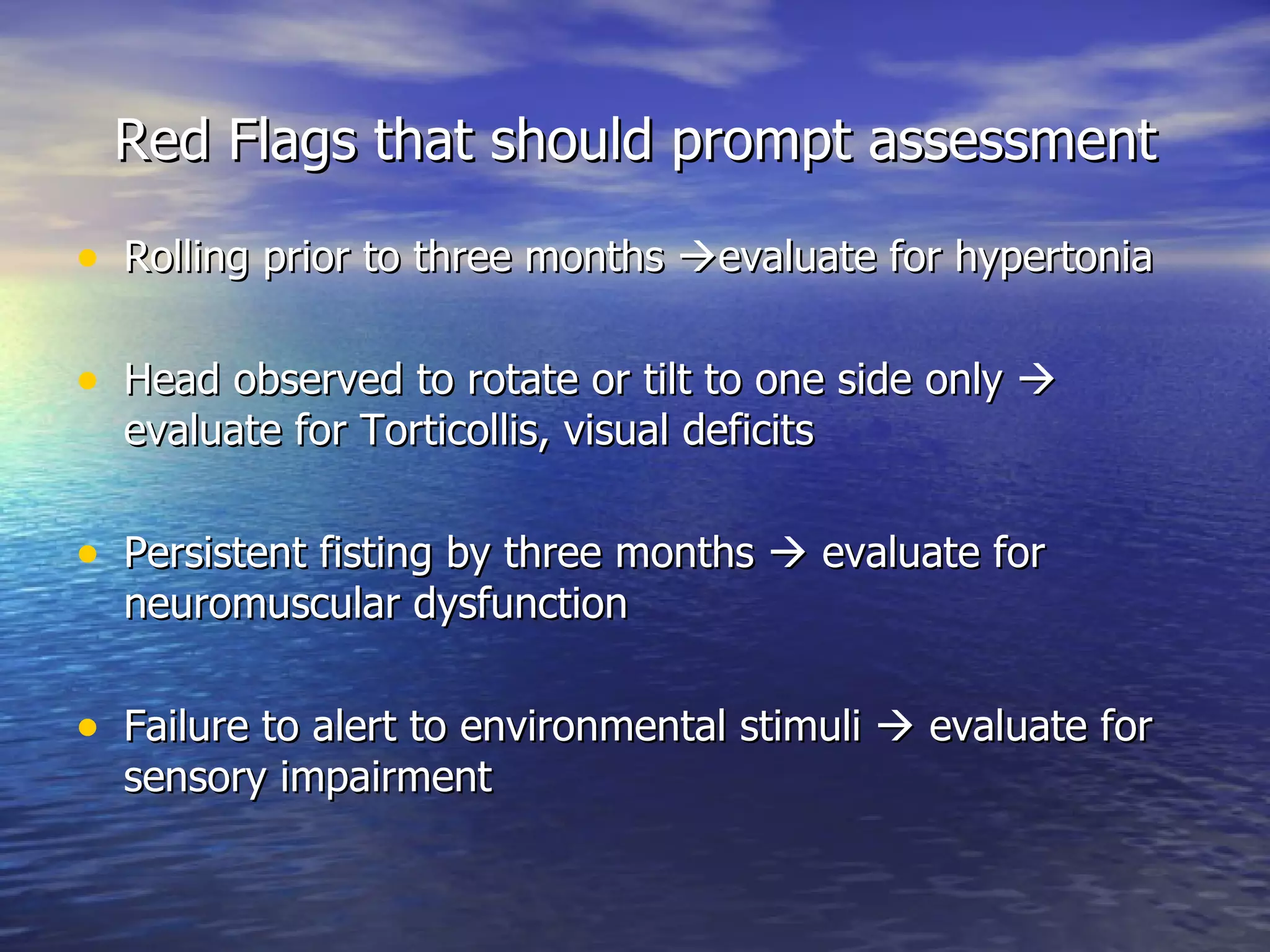
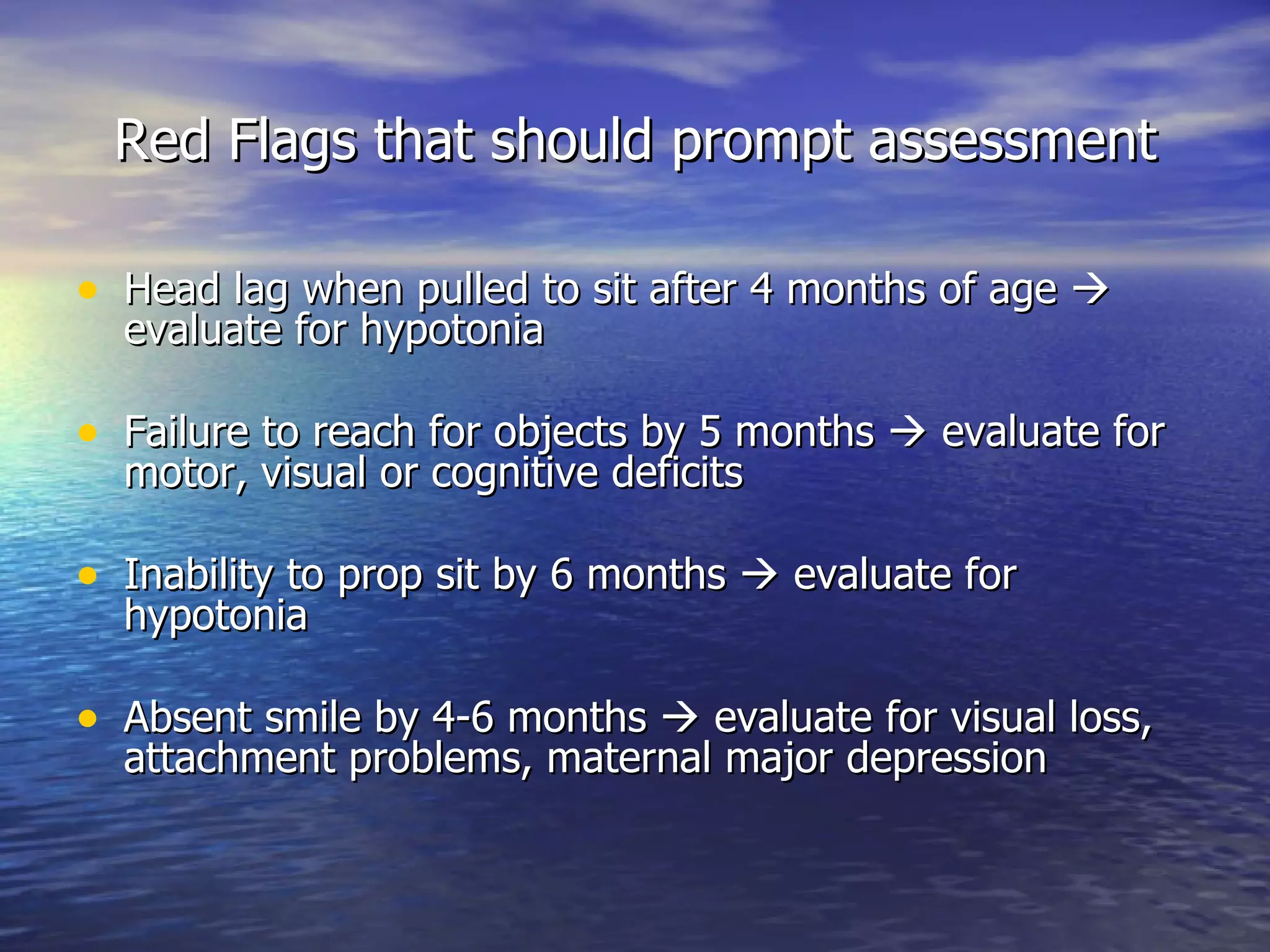
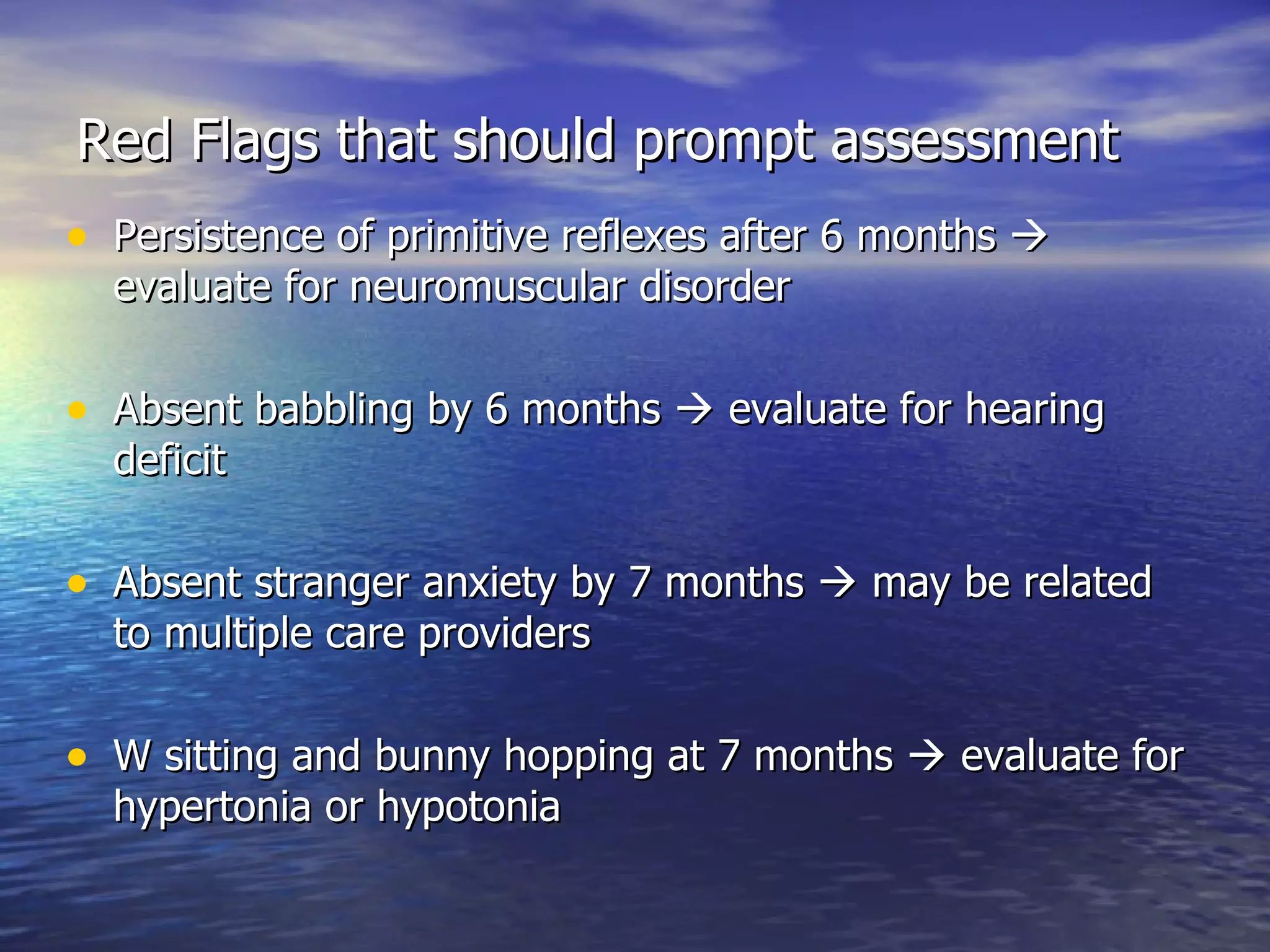
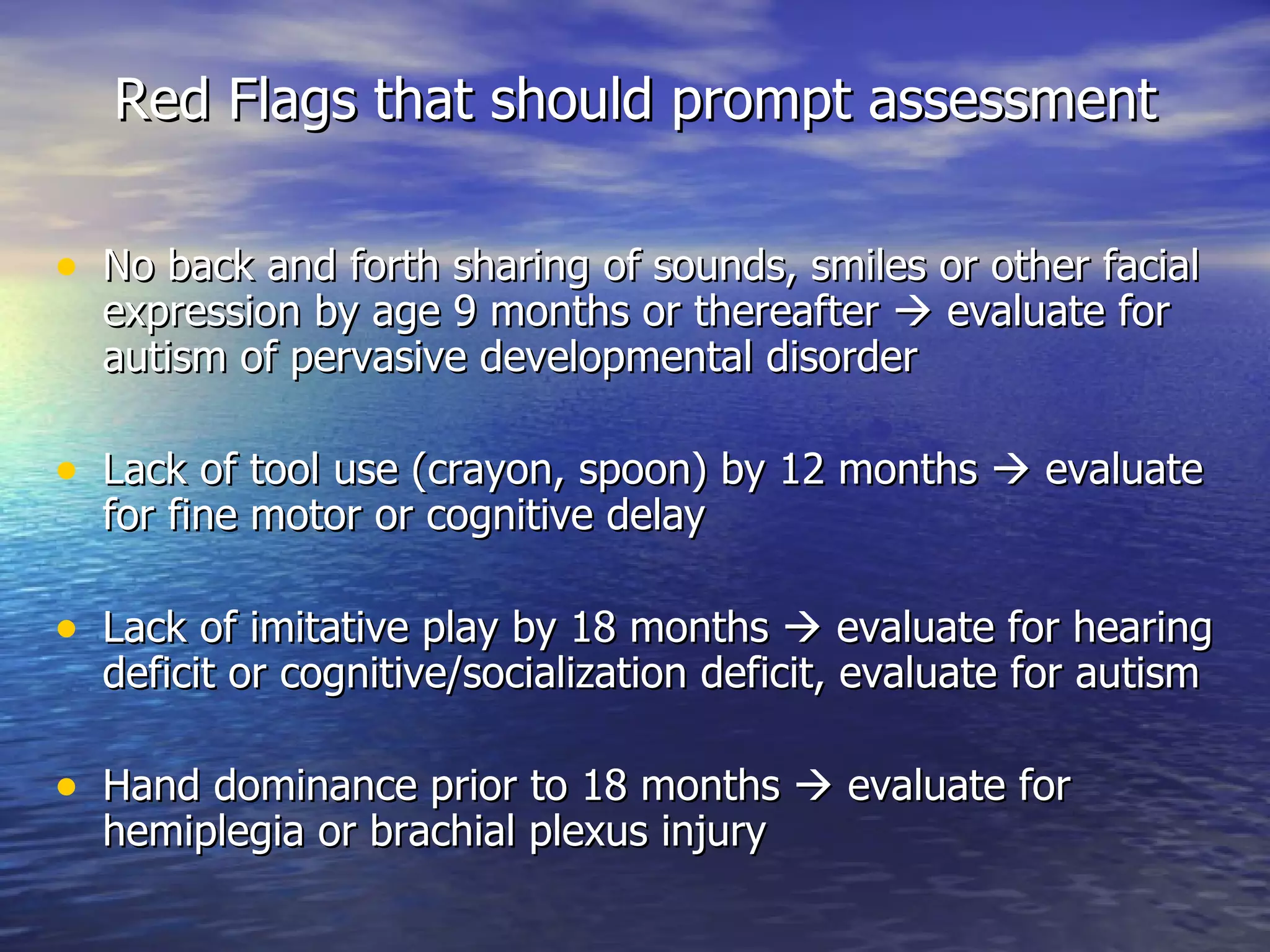
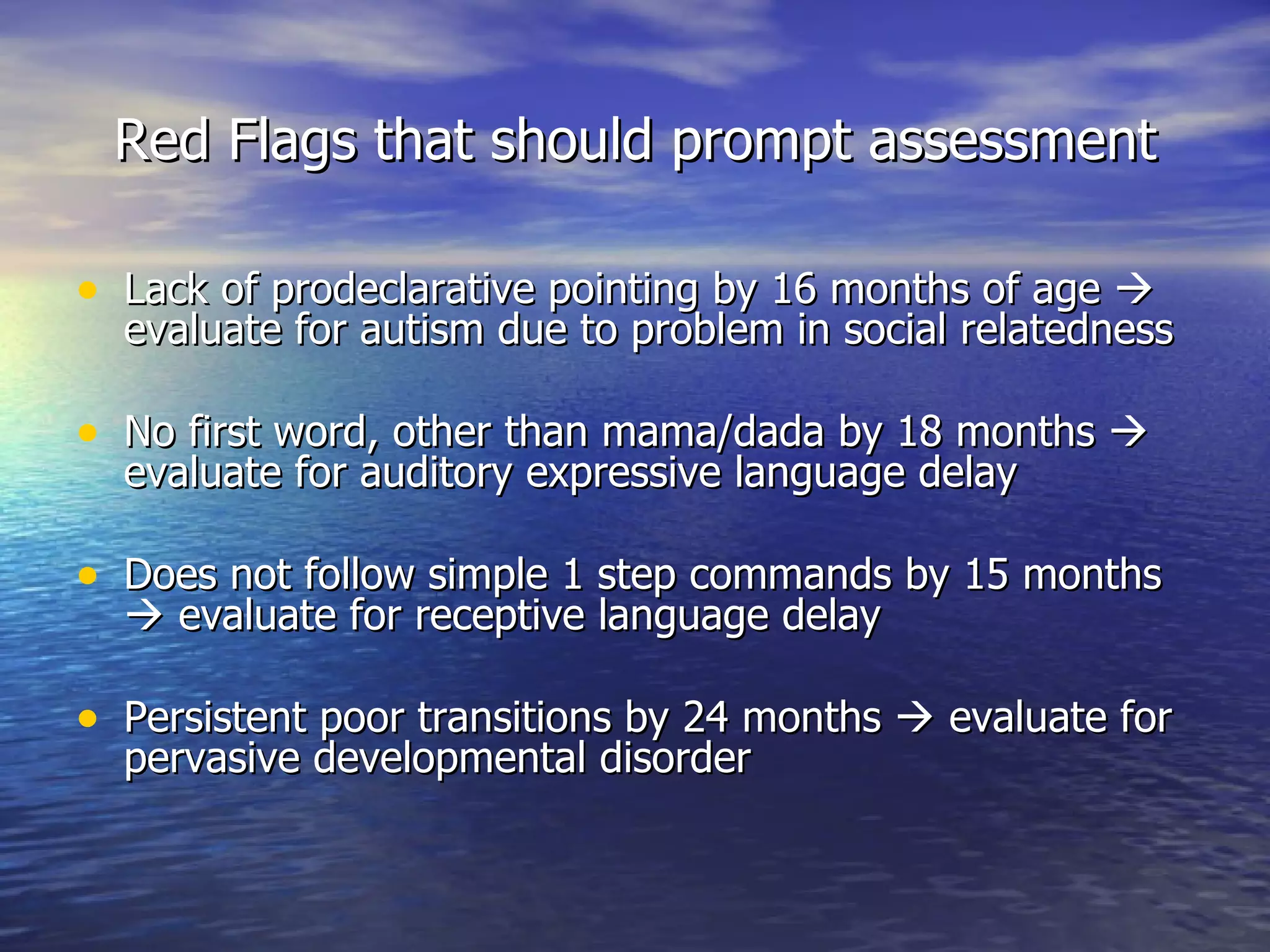
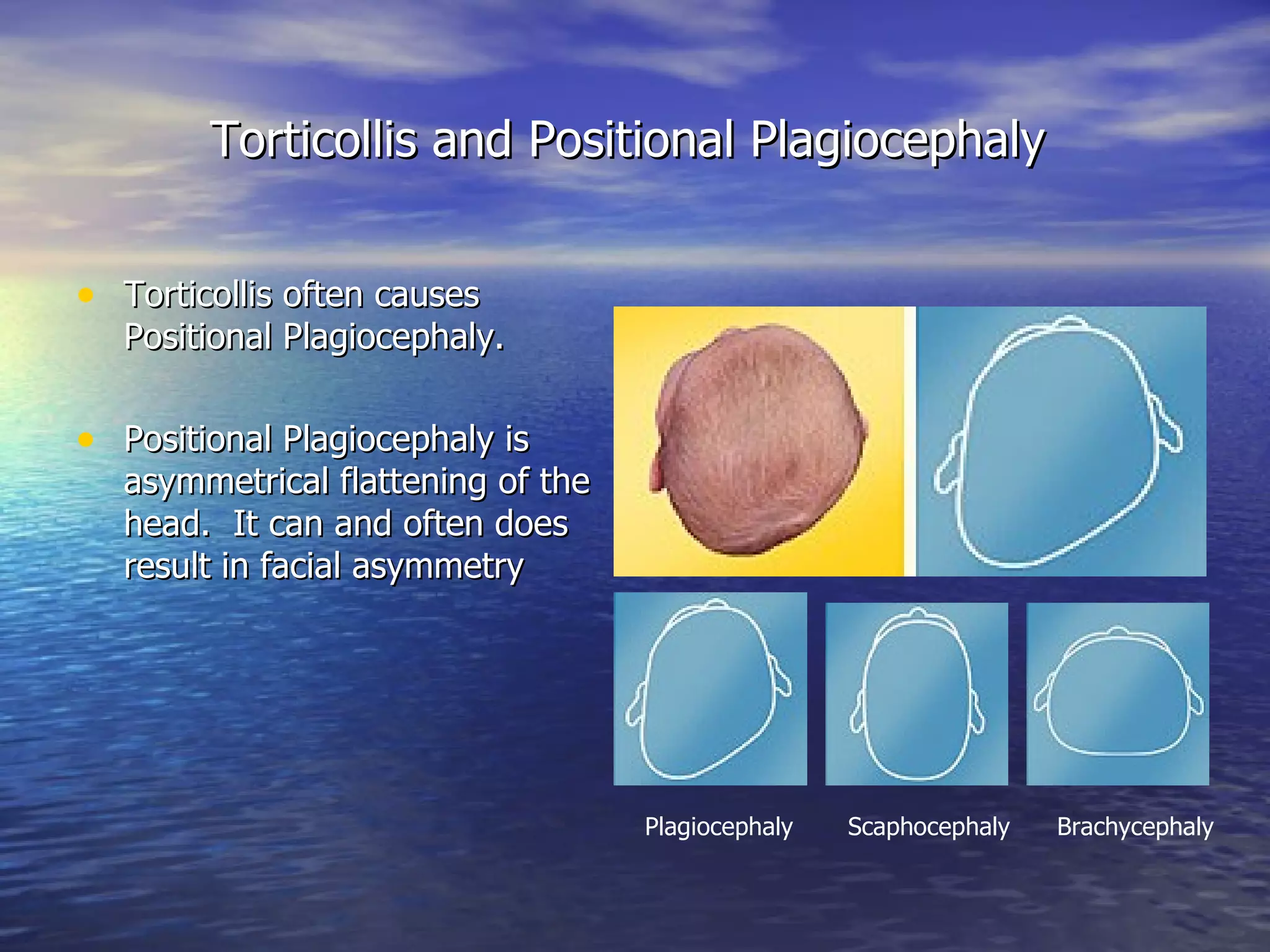
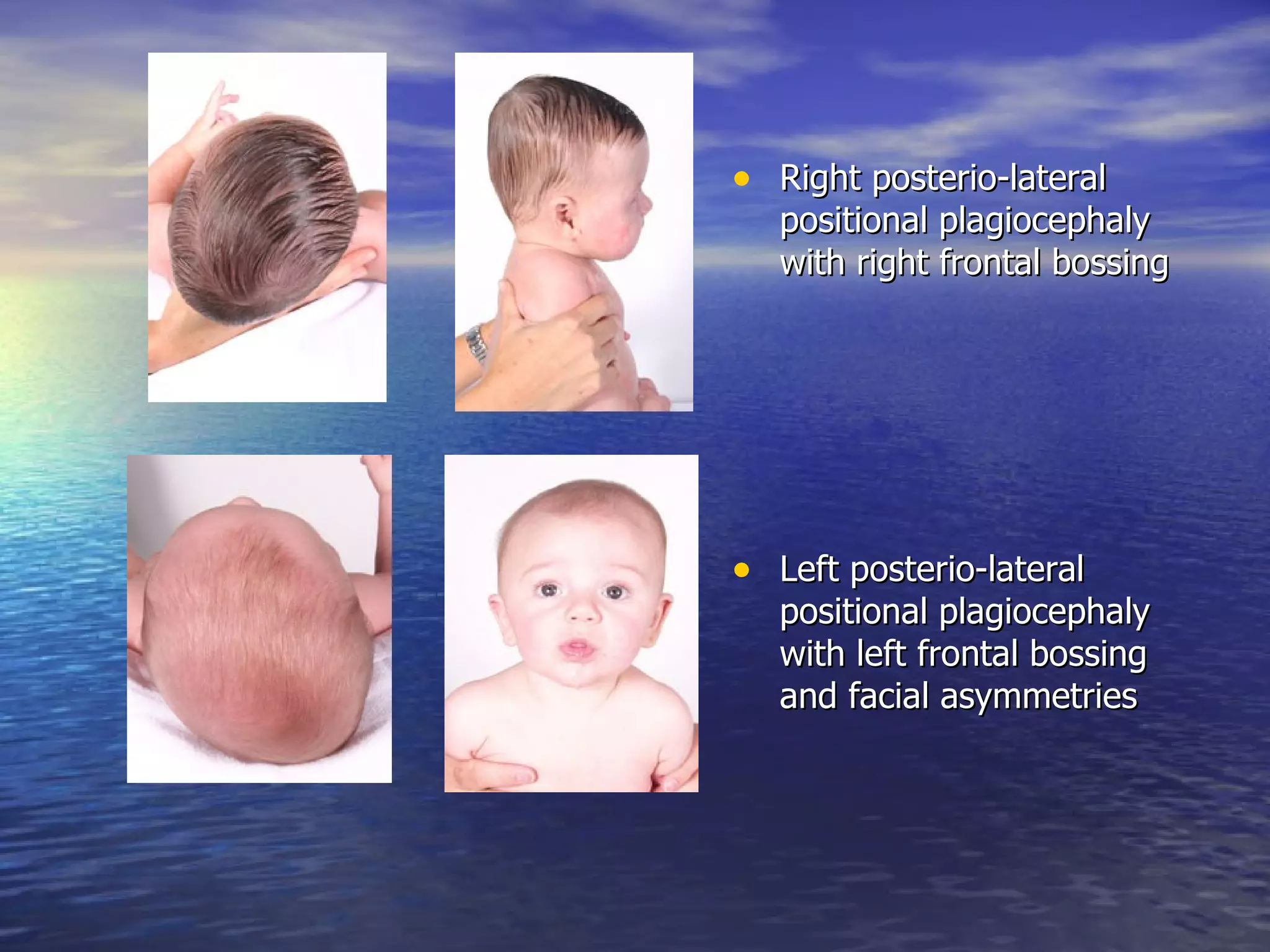
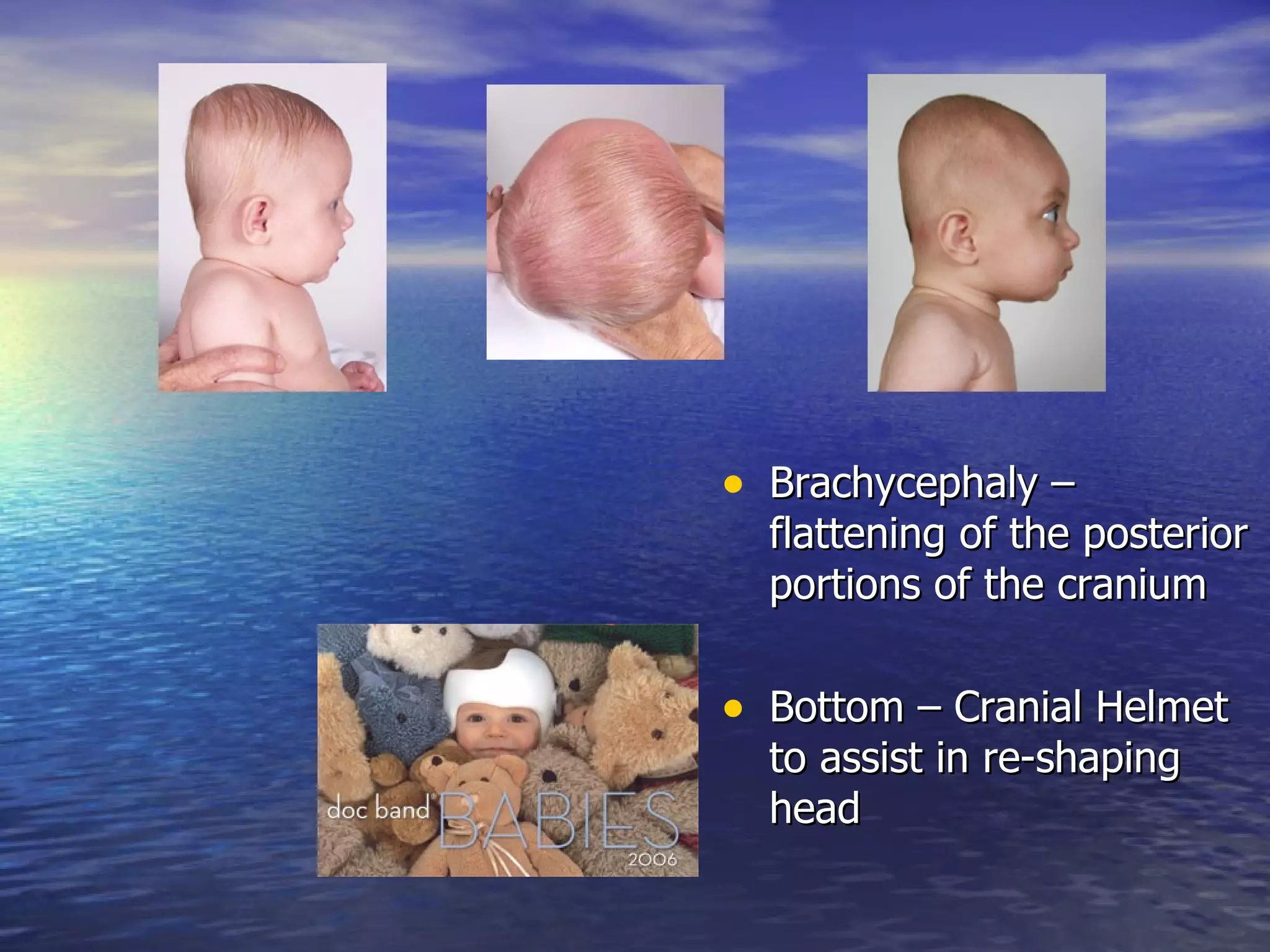
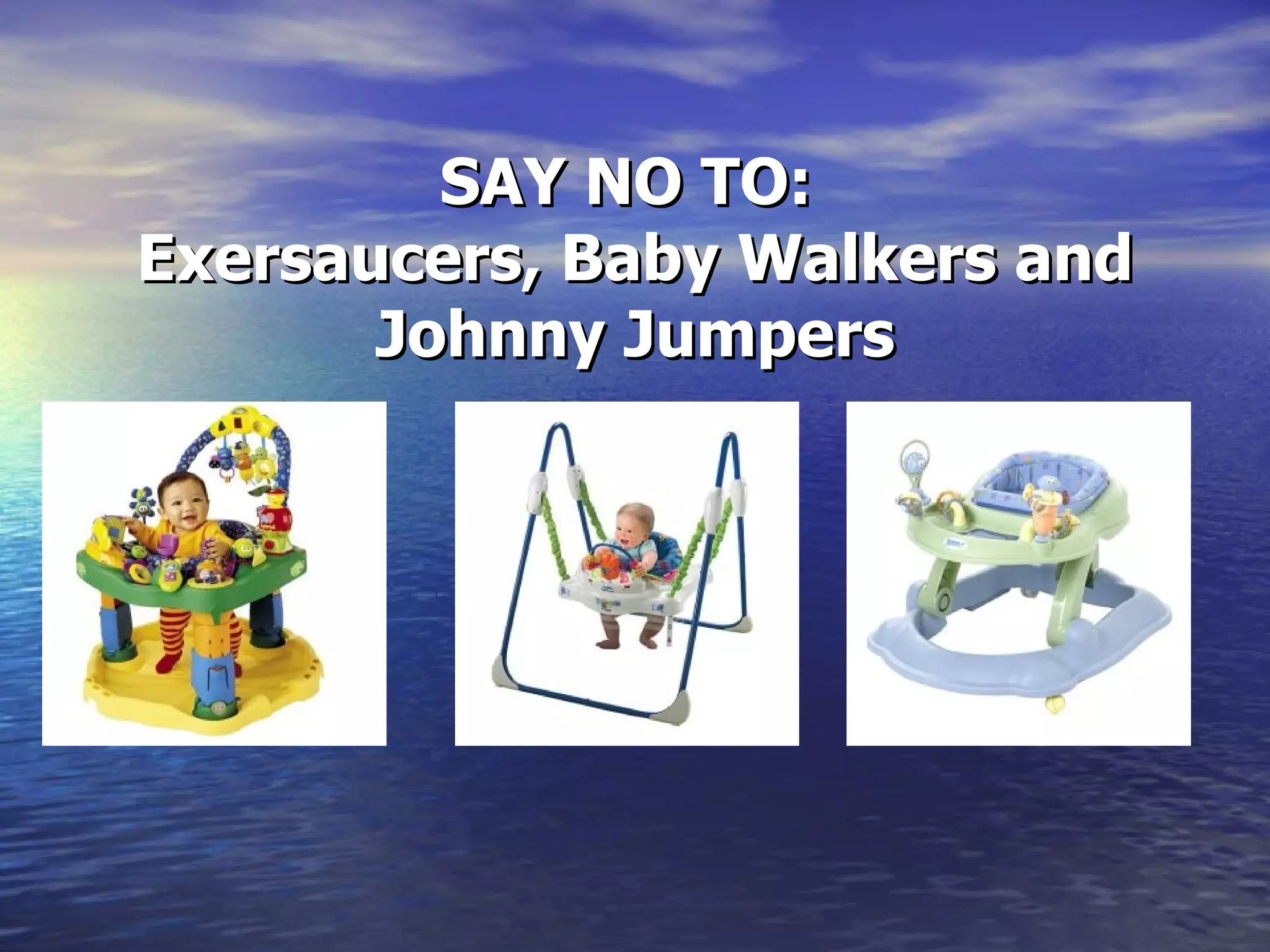
This document provides an overview of typical infant development in the first year. It discusses development milestones for gross motor, fine motor, speech/language skills each month. It also outlines red flags that may indicate atypical development and warrant further assessment by pediatric physical, occupational or speech therapists. These include lack of skills such as head control, sitting, crawling, babbling by certain ages. The document also discusses conditions like torticollis and positional plagiocephaly that should be referred to therapists early for treatment.