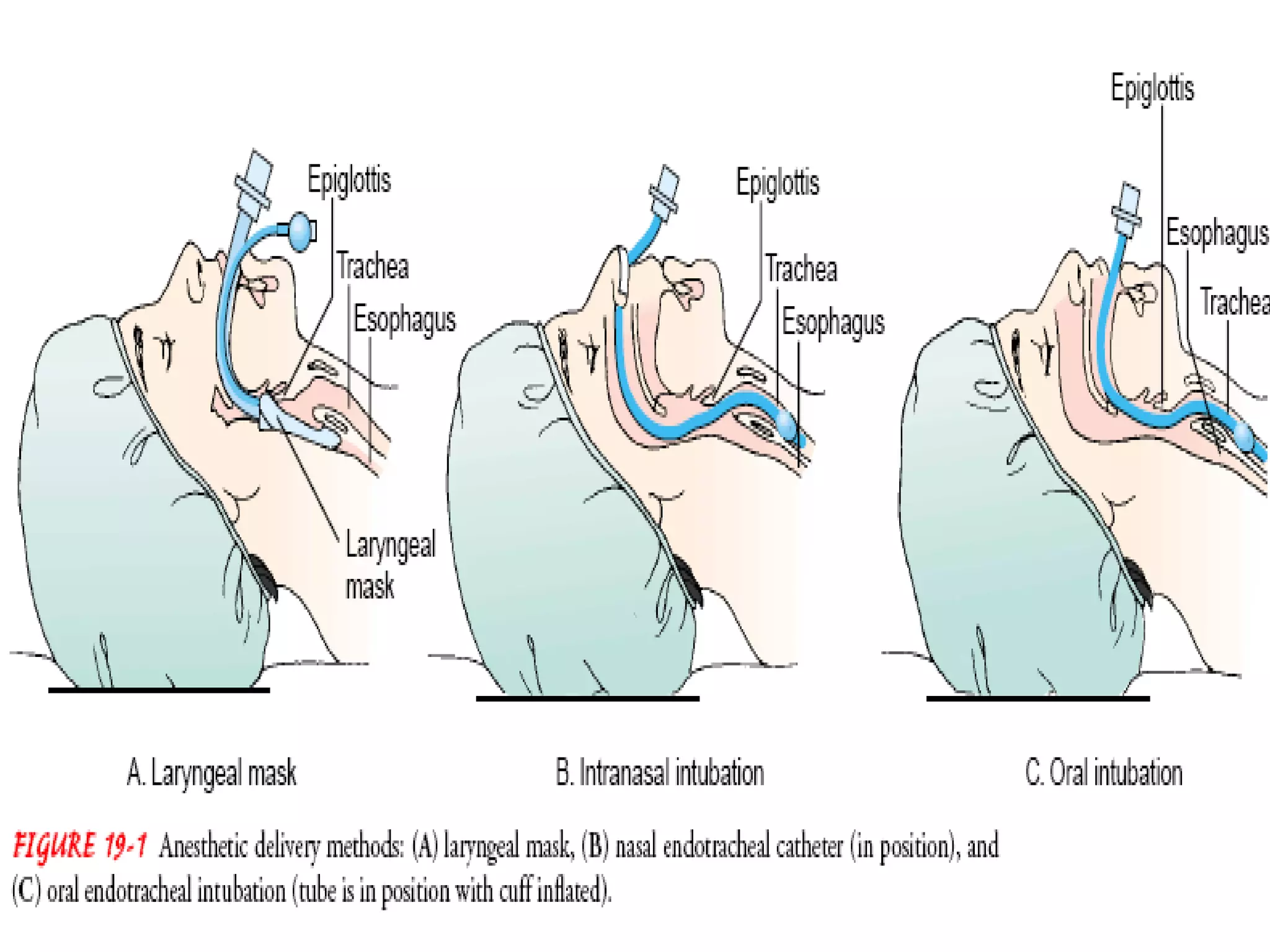
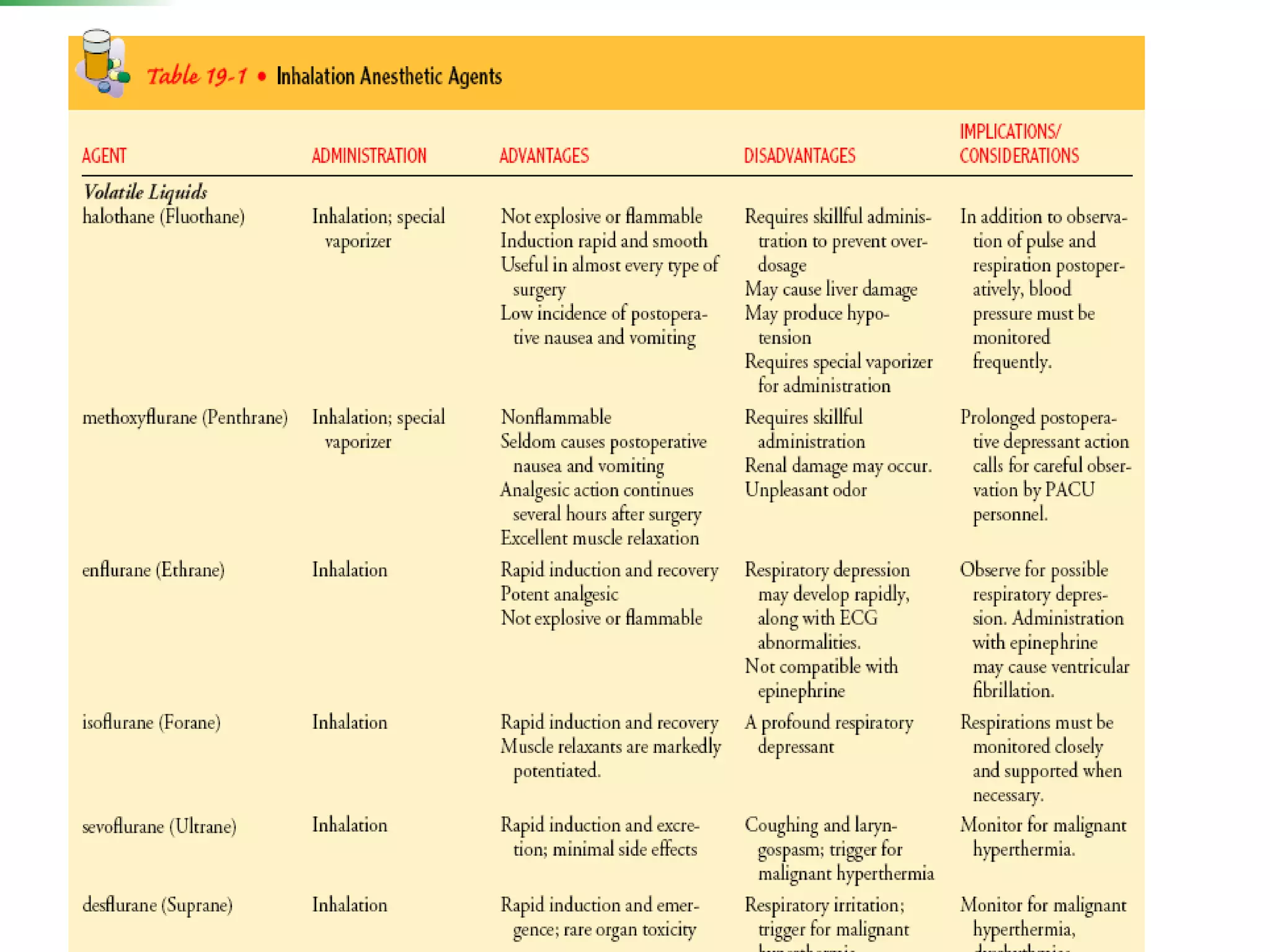
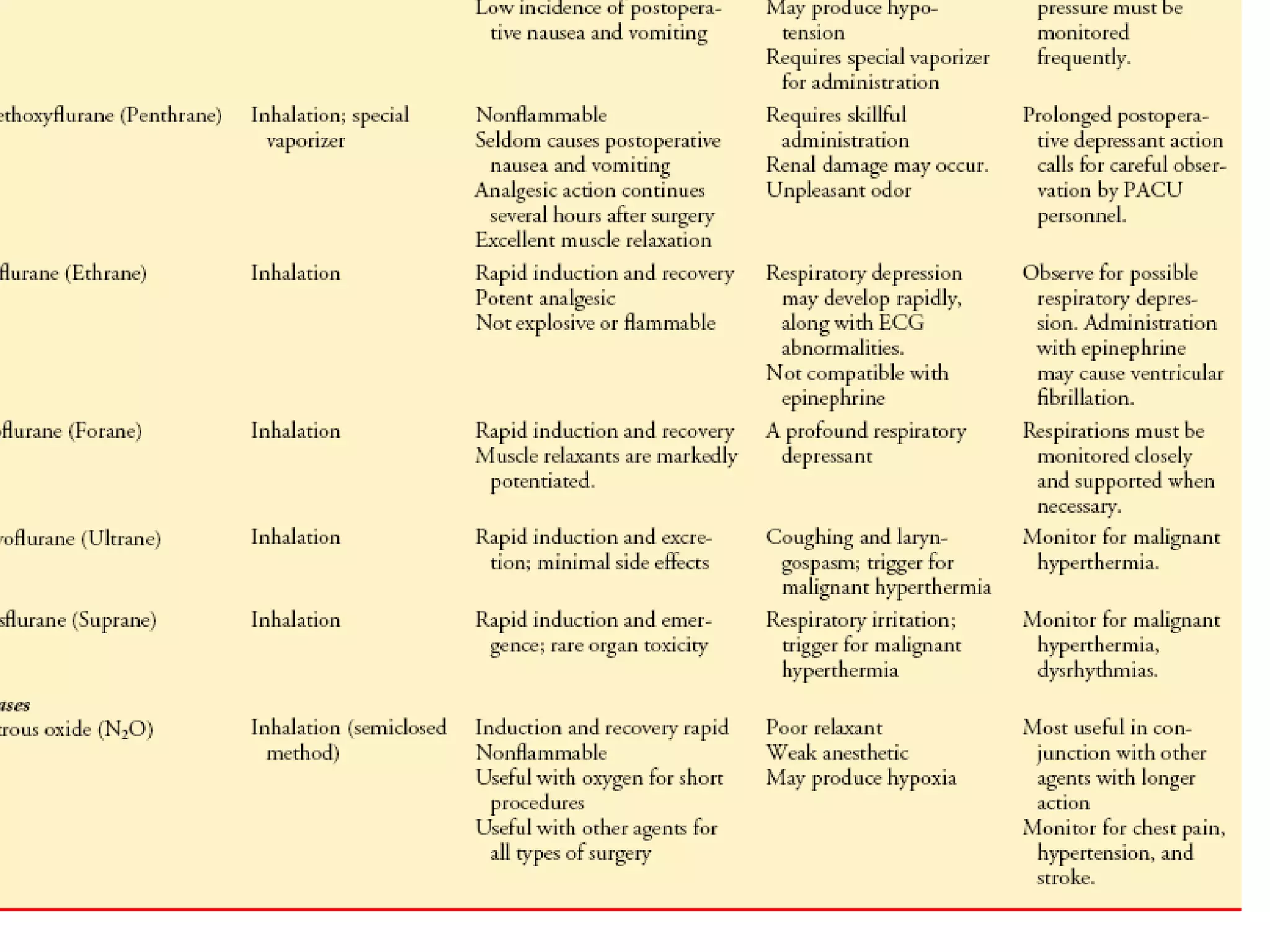
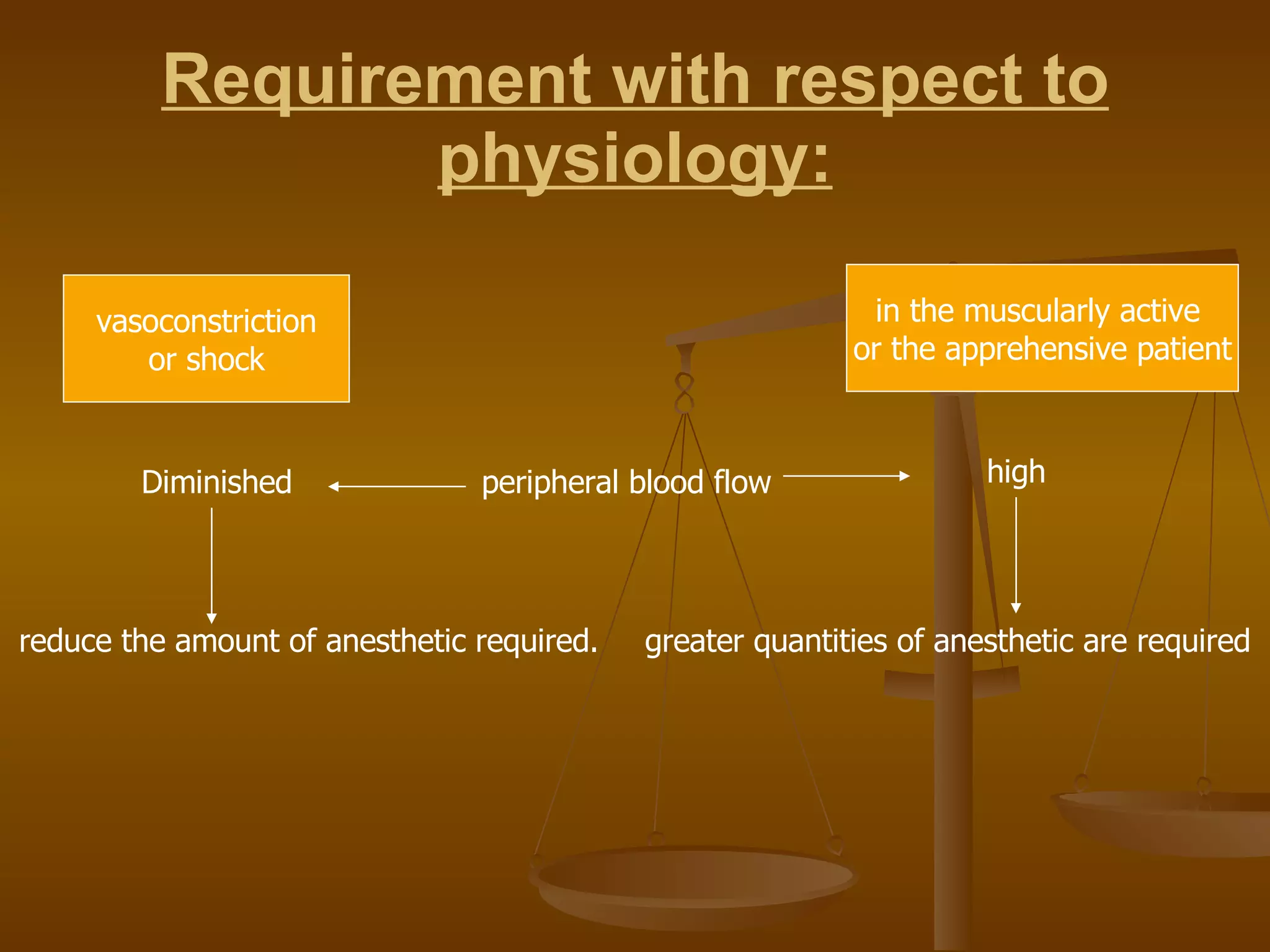
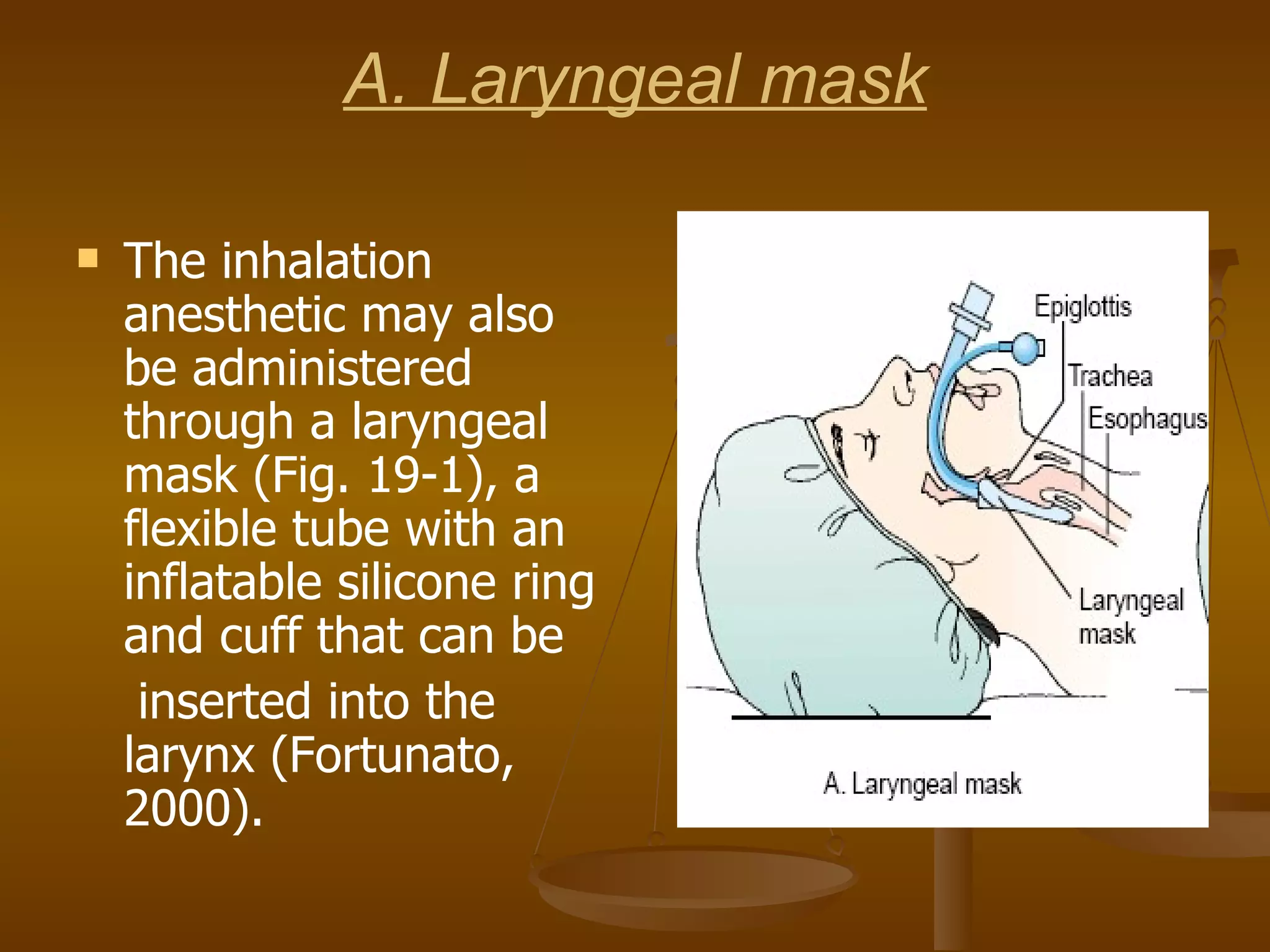
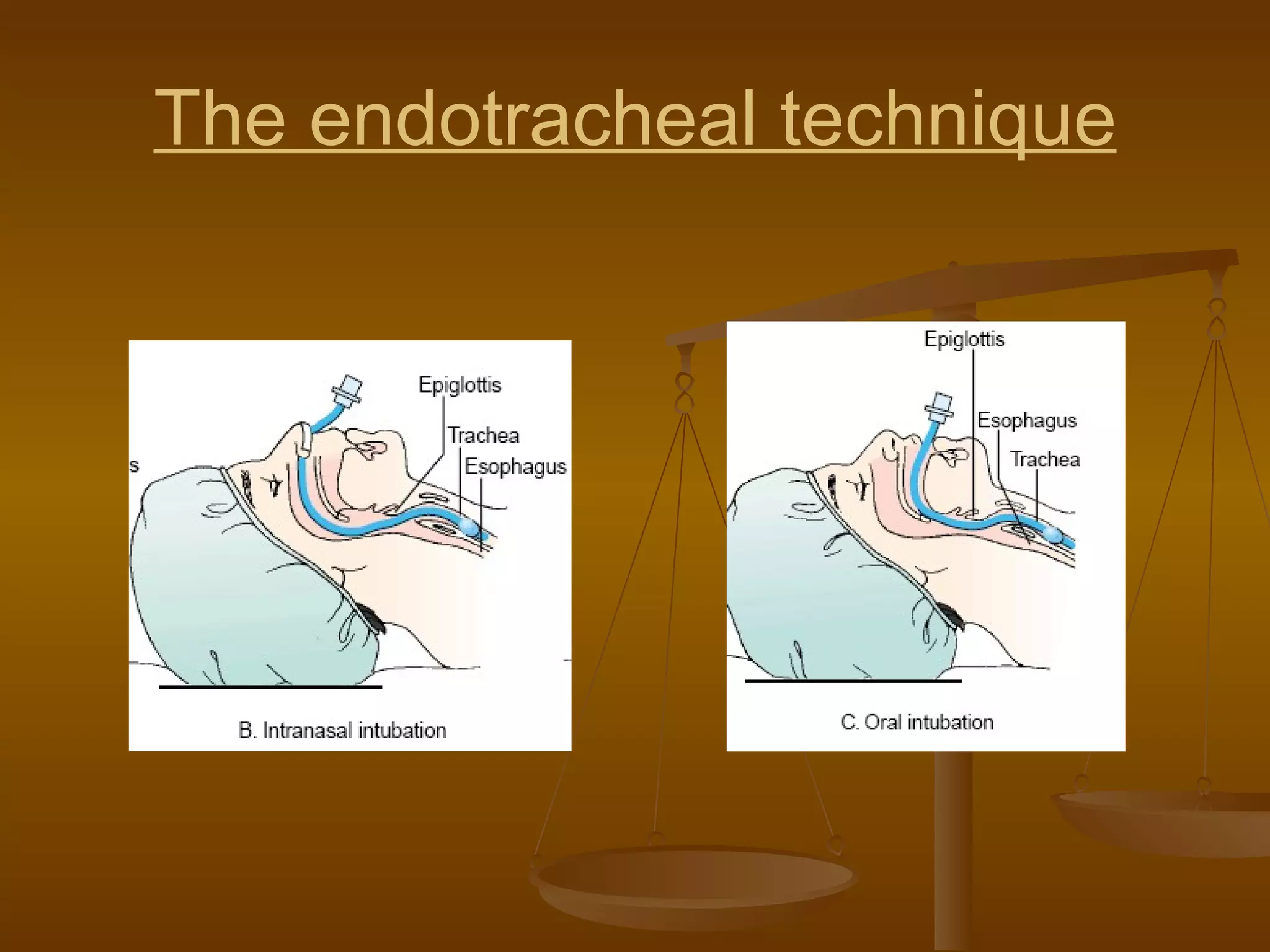
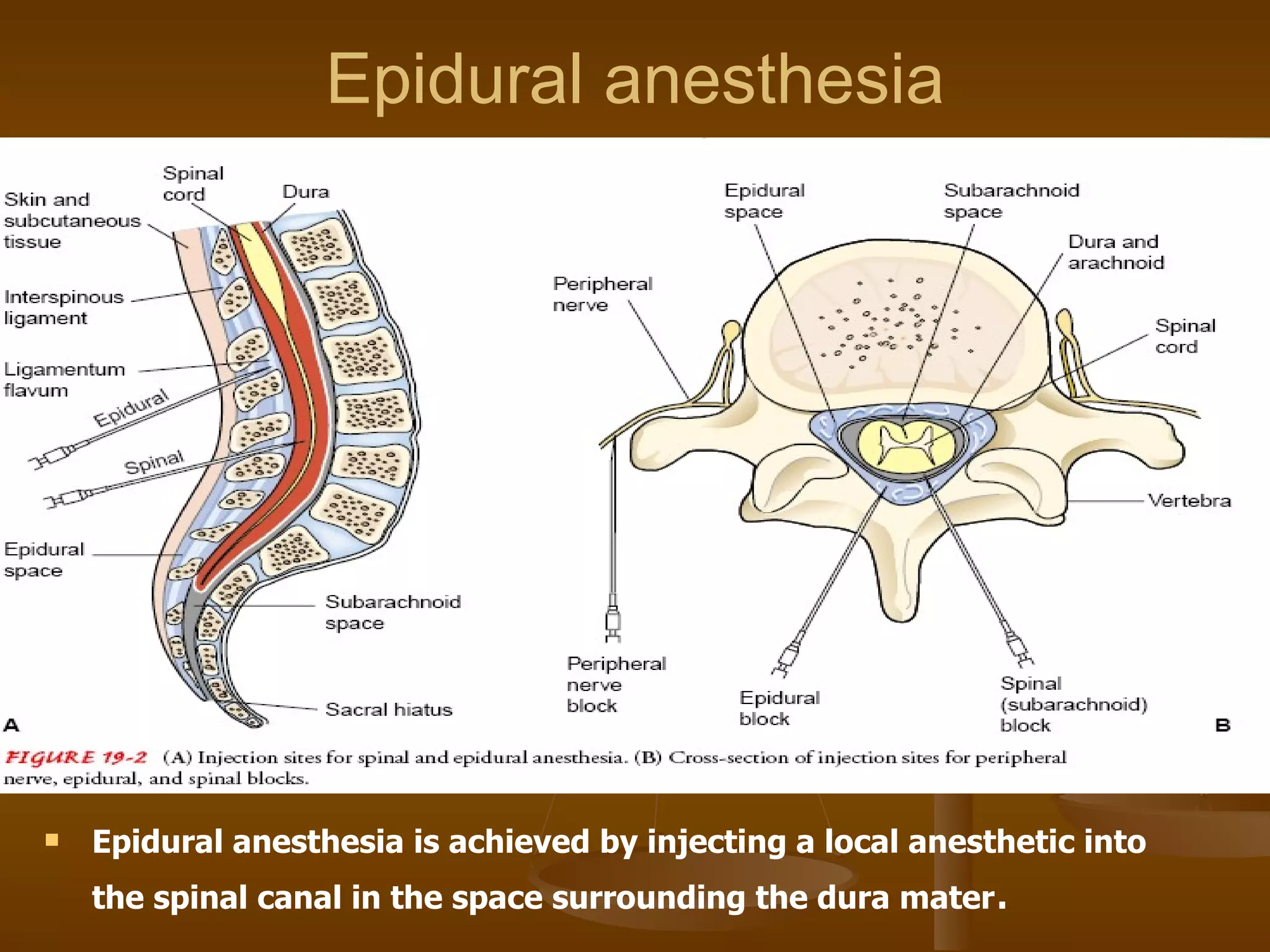
The document summarizes different types of sedation and anesthesia used in surgical procedures. It discusses four levels of sedation from minimal to general anesthesia. It then describes various methods of administering anesthesia including inhalation, intravenous injection, and regional techniques like epidural and spinal anesthesia. The stages of general anesthesia and potential complications are also outlined.