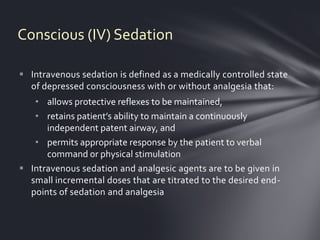
1) Intravenous sedation involves using sedatives and analgesics in small doses to depress consciousness while maintaining breathing and response to commands.
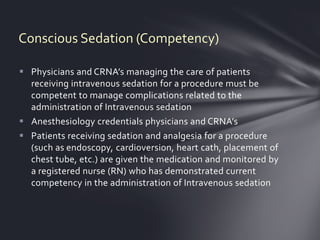
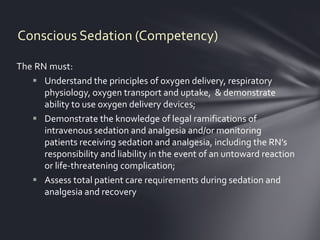
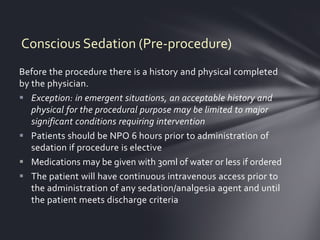
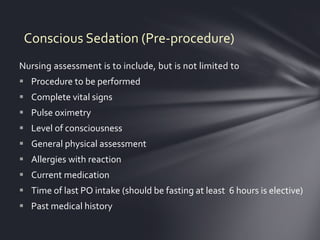
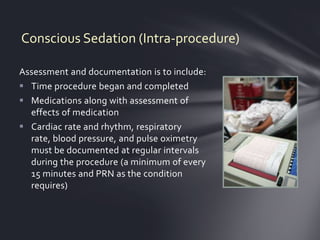
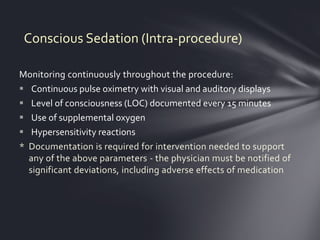
2) Nurses must be competent in administering sedation, including assessing patients before, during, and after procedures while monitoring vitals like breathing and oxygen levels.
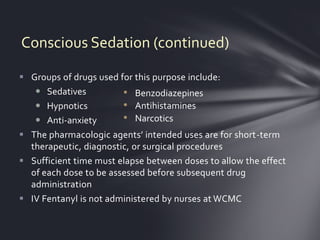
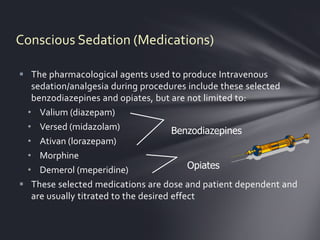
3) The proper equipment and medications must be available in case issues arise during conscious sedation.