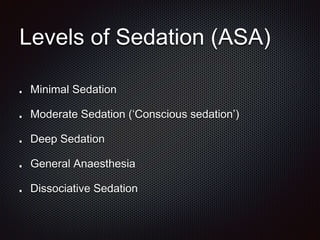
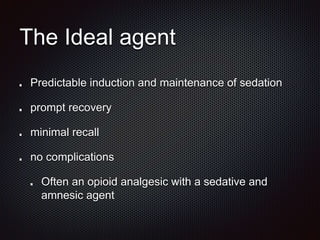
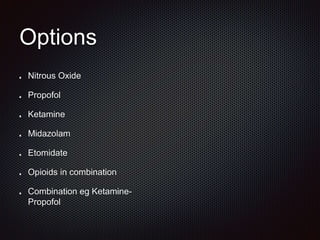
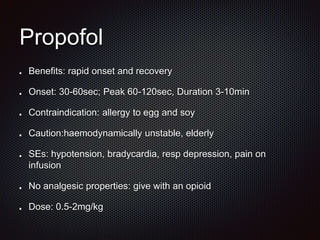
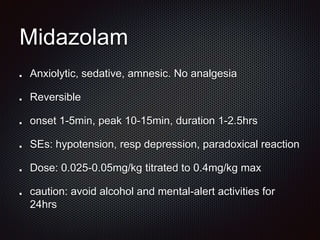
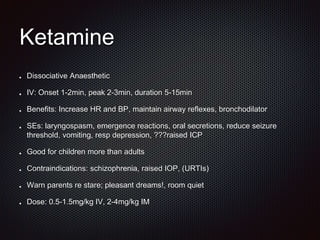
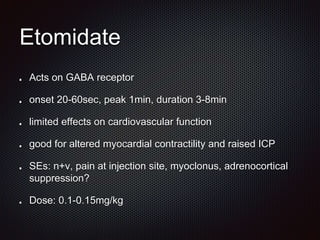
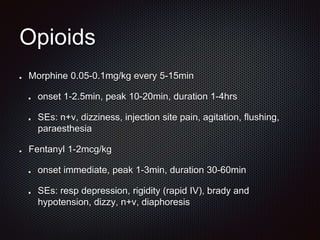
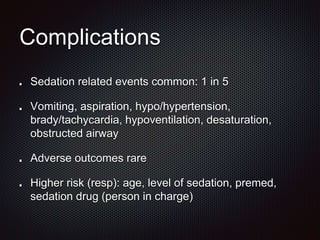
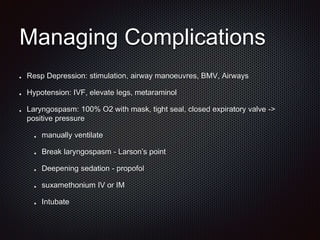
The document discusses procedural sedation, including definitions, common procedures it is used for, advantages over general anesthesia, levels of sedation, ideal agents, options for agents, considerations for assessment, preparation, procedure, aftercare, complications and their management, controversies, and conclusions regarding its importance as an essential emergency medicine skill. Procedural sedation refers to administering sedatives with or without analgesics to allow painful procedures while maintaining cardiorespiratory function. A variety of agents like propofol, ketamine, midazolam, nitrous oxide, and opioids are discussed as options for procedural sedation.





![ReferencesAustralian and New Zealand College of Anaesthetists (ANZCA) (2014) Guidelines on Sedation and/or Analgesia for Diagnostic and
Interventional Medical, Dental or Surgical Procedures. [Online]. Available at: http://www.anzca.edu.au/resources/professional-
documents/pdfs/ps09-2014-guidelines-on-sedation-and-or-analgesia-for-diagnostic-and-interventional-medical-dental-or-surgical-
procedures.pdf (Accessed: 24/3/15).
Bell A, Taylor DM et al. (2011) 'Procedural sedation practices in Australian Emergency Departments', Emergency Medicine
Australasia, 23, pp. 458-465.
Godwin SA, Burton JH et al. (2014) 'Clinical Policy: Procedural Sedation and Analgesia in the Emergency Department', Annals of
Emergency Medicine, 63, pp. 247-258.
Boyle A, Dixon V et al. (2010) 'Sedation of children in the emergency department for short painful procedures compared with
theatre, how much does it save? Economic evaluation', Emergency Medicine Journal, 28, pp. 383-386.
Andolfatto G, Abu-Laban RB et al (2012) 'Ketamine-Propofol Combination (Ketofol) Versus Propofol Alone for Emergency
Department Procedural Sedation and Analgesia: A Randomized Double-Blind Trial', Annals of Emergency Medicine, 59(6), pp. 504-
512.
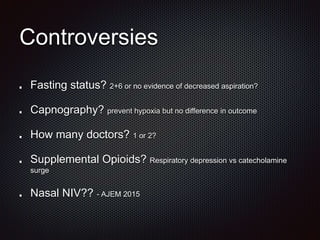
Miner JR, Moore JC et al (2013) 'Randomized Clinical Trial of the Effect of Supplemental Opioids in Procedural Sedation with
Propofol on Serum Catecholamines', Academic Emergency Medicine, 20(4), pp. 330-337.
Strayer RJ, Caputo ND (2015) 'Noninvasive ventilation during procedural sedation in the ED: a case series', American Journal of
Emergency Medicine, 33, pp. 116-120.
Taylor DM, Bell A et al. (2011) 'Risk factors for sedation-related events during procedural sedation in the emergency department',
Emergency Medicine Australasia , 23(), pp. 466-473.](https://image.slidesharecdn.com/proceduralsedation-150407214028-conversion-gate01/85/Procedural-Sedation-29-320.jpg)