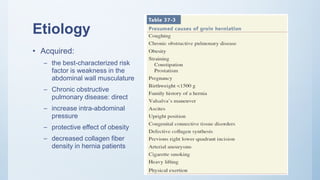
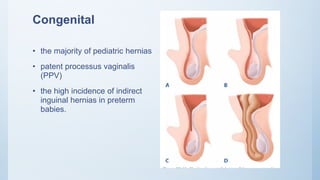
1. Inguinal hernia repair is the most common operation performed in the United States, with 75% of abdominal wall hernias occurring in the groin region. Inguinal hernias are more common in males, with a peak incidence before age 1 and after age 40.
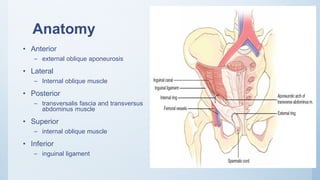
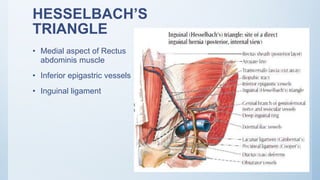
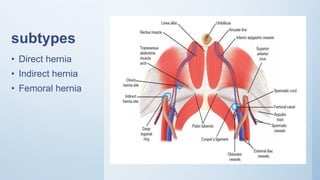
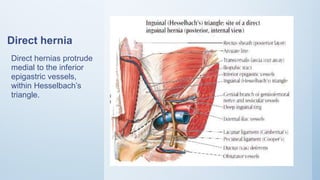
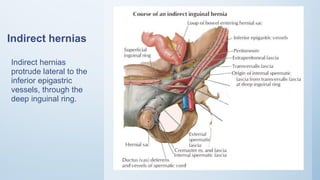
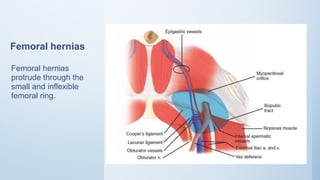
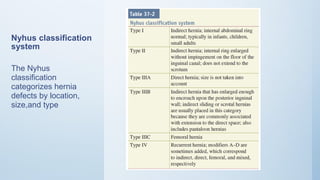
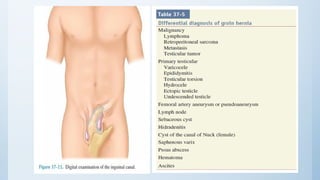
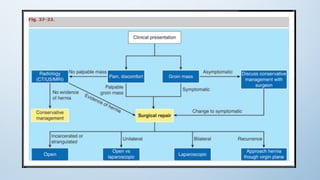
2. Inguinal hernias can be direct, indirect, or femoral based on their anatomical location. Surgical repair with mesh is the definitive treatment, while conservative management with trusses is not recommended due to risk of complications.
3. Incarcerated or strangulated hernias require emergent surgery, while asymptomatic or minimally symptomatic hernias can often be initially managed non-oper