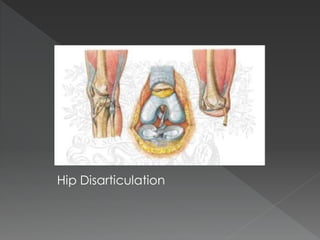
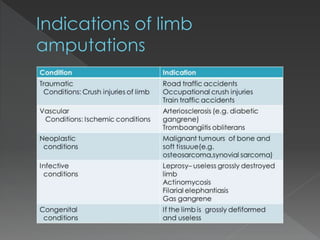
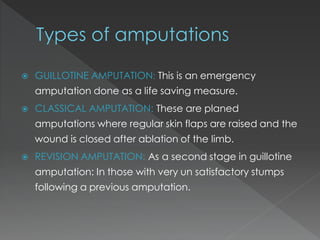
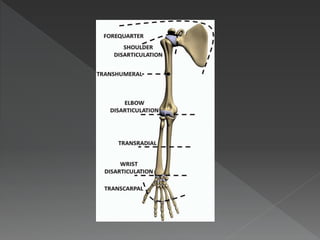
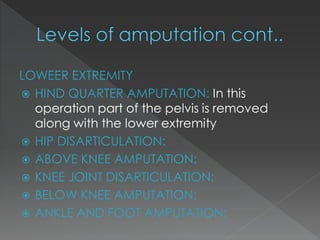
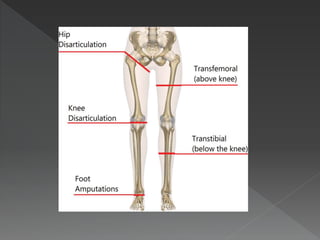
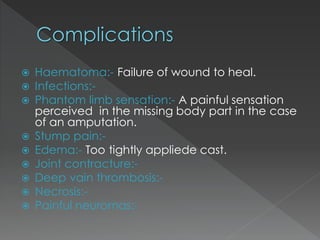
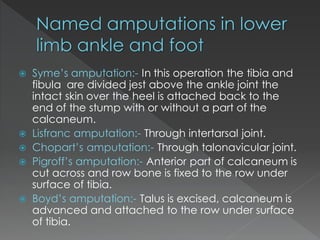
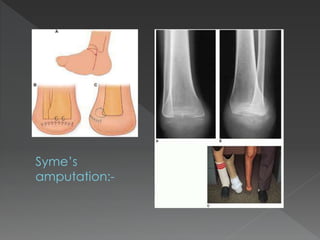
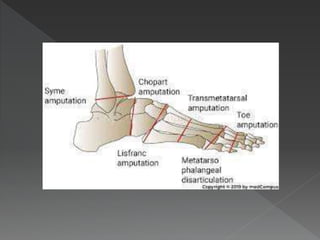
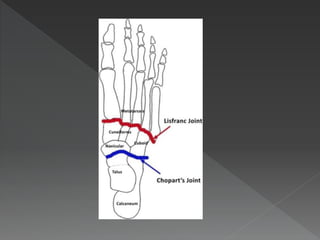
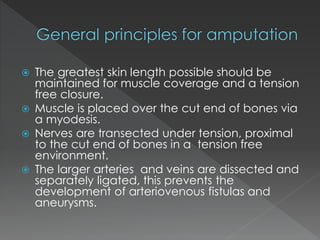
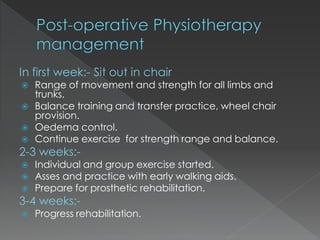
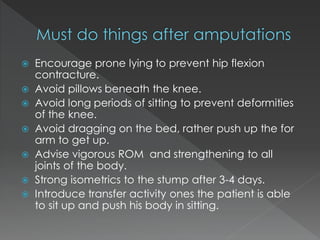
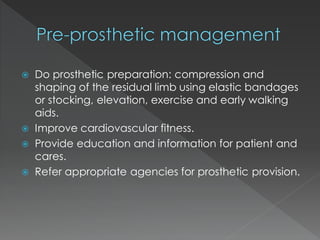
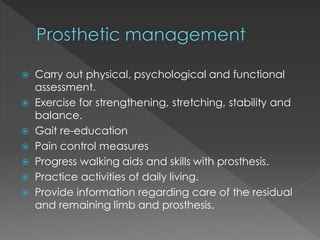
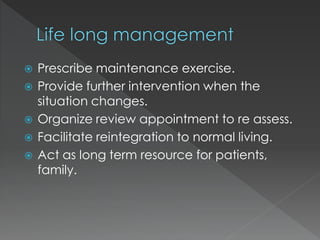
Amputation is the surgical removal of part or all of a limb. It should only be considered if the limb is dead, dying, dangerous, or useless. There are several types of amputations for both upper and lower limbs depending on the level and joint removed. Proper rehabilitation after amputation includes wound care, stump exercises, mobility training, prosthetic fitting and gait re-education to help the patient regain function.