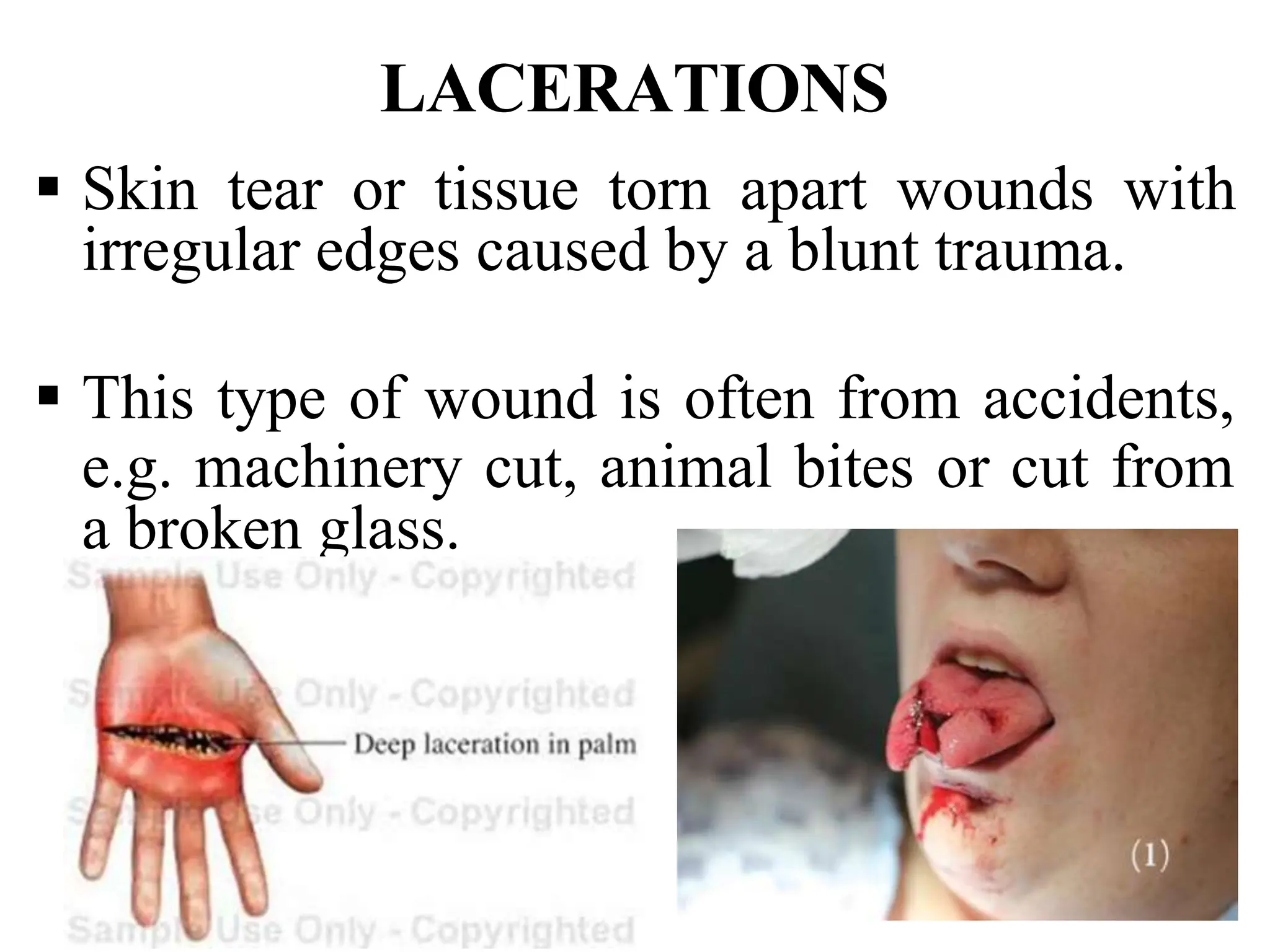
This document provides an overview of wound classification and the wound healing process. It begins with the objectives and defines a wound. It then classifies wounds according to surface covering, depth of injury, cause, type of injury, and degree of contamination. The stages of wound healing are described as inflammatory, proliferative, and maturation phases. Key processes in the proliferative phase include granulation, wound contraction, and epithelialization which work to fill the wound with new tissue and close it.