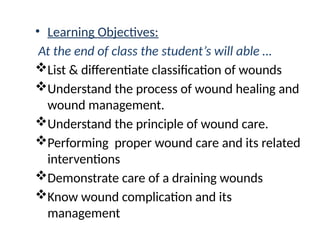
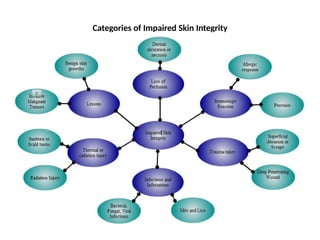
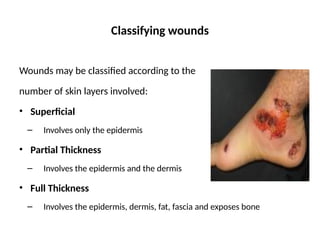
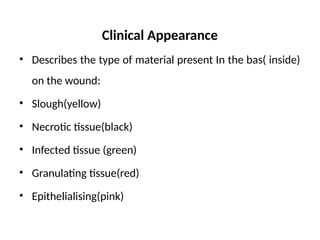
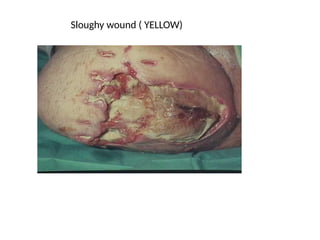
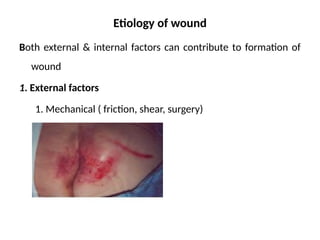
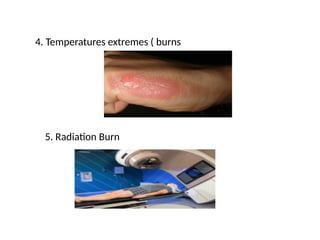
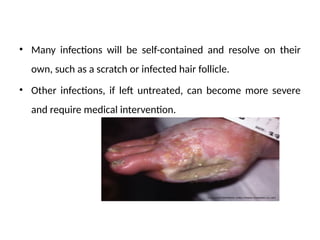
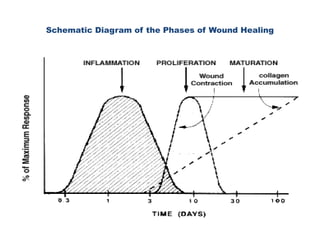
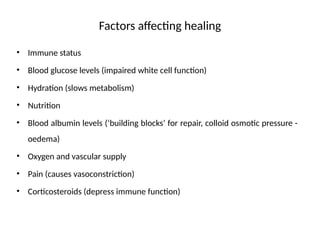
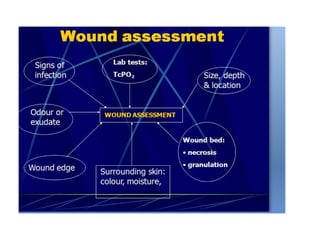
The document covers basic wound care principles, including classification of wounds, the wound healing process, and complications associated with wound management. It highlights the importance of proper wound assessment, categorizing different wound types, and the three phases of wound healing: inflammatory, proliferative, and maturation. Practical considerations for care and factors affecting healing outcomes, such as nutrition and infection control, are also discussed.






![Foot care cont…
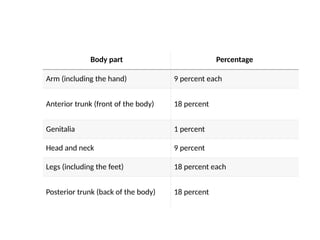
• If your feet are an abnormal shape, or other foot problems, you may
need specially fitted shoes to stop your feet rubbing.
• Tips to avoid foot burns include: checking the bath temperature with
your hand before stepping in; do not use hot water bottles, do not sit too
close to fires.
• Sammary on health education
• 1. teach about foot care 3. teach about medication
• 2 teach about dalily exercise 4. about diet 5. about RBS [low blood
glucose s/sx]](https://image.slidesharecdn.com/basicwoundcare-241112072805-f9e3f7da/85/basic-wound-care-for-nursing-students-pptx-AD-pptx-104-320.jpg)
![Superficial (First degree)
• Layers involved Epidermis
• Appearance Red without blisters]
• Texture Dry
• Sensation Painful
• Prognosis Heal well; Repeated the risk of skin cancer later in
life](https://image.slidesharecdn.com/basicwoundcare-241112072805-f9e3f7da/85/basic-wound-care-for-nursing-students-pptx-AD-pptx-120-320.jpg)





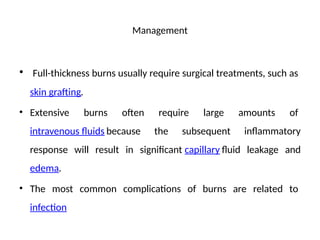
![Management
• This is followed by care of the burn wound itself.
• People with extensive burns may be wrapped in clean sheets
until they arrive at a hospital.
• As burn wounds are prone to infection, a tetanus booster shot
should be given if an individual has not been immunized
within the last five [5] years.](https://image.slidesharecdn.com/basicwoundcare-241112072805-f9e3f7da/85/basic-wound-care-for-nursing-students-pptx-AD-pptx-146-320.jpg)
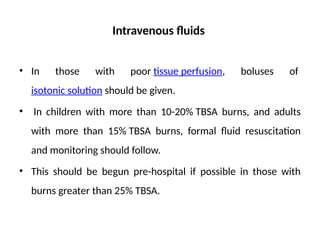
![Intravenous fluids
• In those with poor tissue perfusion, boluses of isotonic crystalloid solution
For example [Lactated Ringer’s—[R/L]
• An isotonic crystalloid solution containing the solutes sodium chloride, potassium chloride,
calcium chloride, and sodium lactate, dissolved in sterile water (solvent).]should be given.
• In children with more than 10-20% TBSA burns, and adults with more
than 15% TBSA burns, formal fluid resuscitation and monitoring should
follow.](https://image.slidesharecdn.com/basicwoundcare-241112072805-f9e3f7da/85/basic-wound-care-for-nursing-students-pptx-AD-pptx-150-320.jpg)