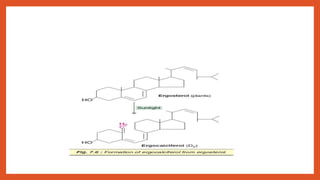
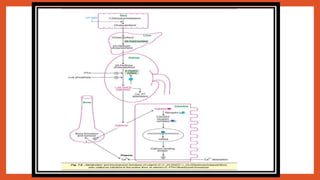
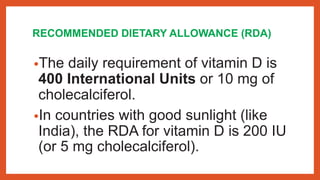
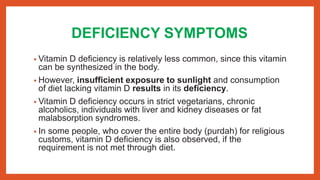
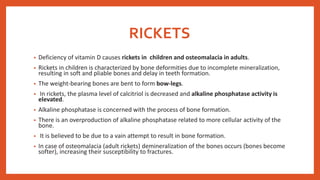
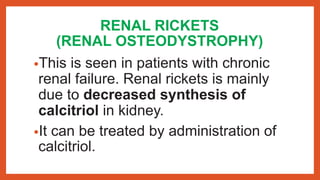
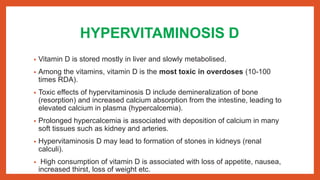
Vitamin D is a fat-soluble vitamin essential for calcium and phosphate absorption, found in two forms: ergocalciferol (D2) from plants and cholecalciferol (D3) from animals. It is synthesized in the skin upon sunlight exposure and regulated by calcium and phosphate levels, impacting functions in the intestine, bone, and kidney. Deficiency can lead to conditions like rickets, while excess can cause hypervitaminosis D and its toxic effects.