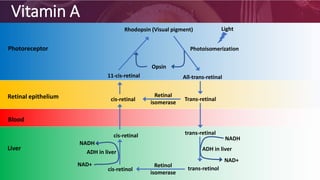
The document discusses the classification, biological functions, deficiencies, and sources of fat-soluble vitamins (A, D, E, and K) and water-soluble vitamins (B complex and C). It details the absorption, storage, and toxicities associated with fat-soluble vitamins, with specific focus on the health implications of deficiencies, particularly of vitamin A, D, and K. Additionally, it highlights the importance of these vitamins in various physiological processes, including vision, bone health, and blood coagulation.