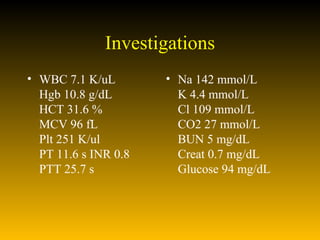
1. A 29-year-old woman experienced sudden loss of vision in her right eye and worsening neck pain after undergoing cervical manipulation by her chiropractor.
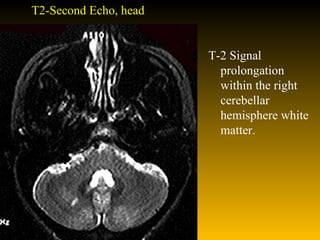
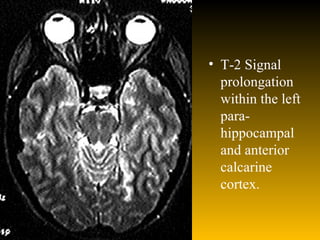
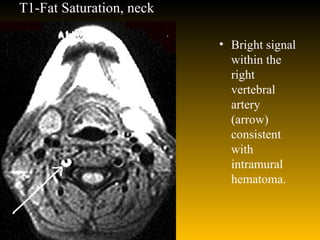
2. MRI revealed a right cerebellar hemisphere infarct and a left mesial temporal infarct, as well as a signal within the right vertebral artery consistent with an intramural hematoma.
3. She was diagnosed with vertebral artery dissection causing distal posterior circulation embolization and stroke. The manipulation likely dislodged a clot from a pre-existing vertebral artery dissection.