1. Stroke occurs when the blood supply to the brain is reduced or blocked, preventing brain tissue from receiving oxygen and nutrients.
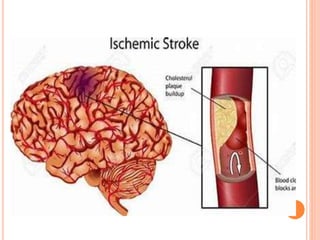
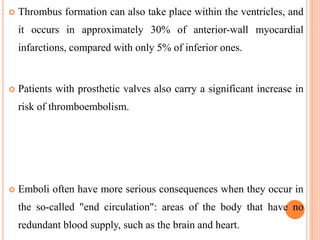
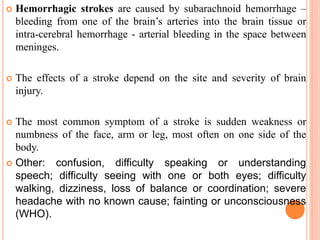
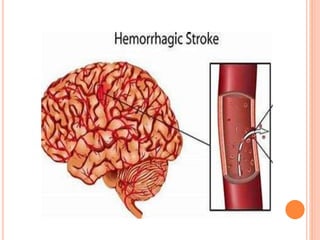
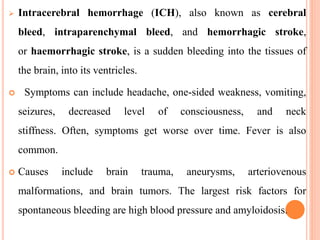
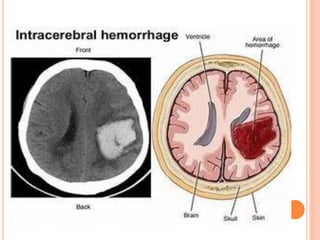
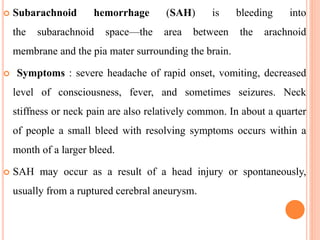
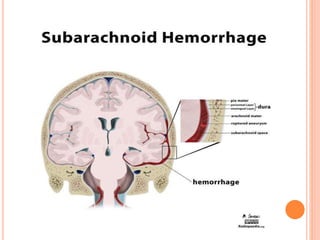
2. Strokes are classified as either ischemic (caused by blockage of arteries) or hemorrhagic (caused by bleeding in or around the brain).
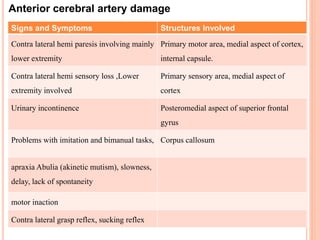
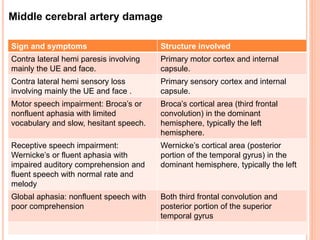
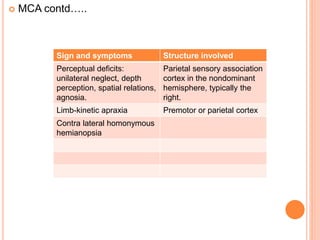
3. Common symptoms of stroke include sudden weakness or numbness on one side of the body, difficulty speaking, confusion, and severe headache. Early recognition and treatment are important to reduce long-term disability.