- A ventricular septal defect (VSD) is a hole in the wall separating the two lower chambers of the heart, known as the ventricular septum.
- VSDs are among the most common types of congenital heart defects, occurring in 3-5 per 1000 live births.
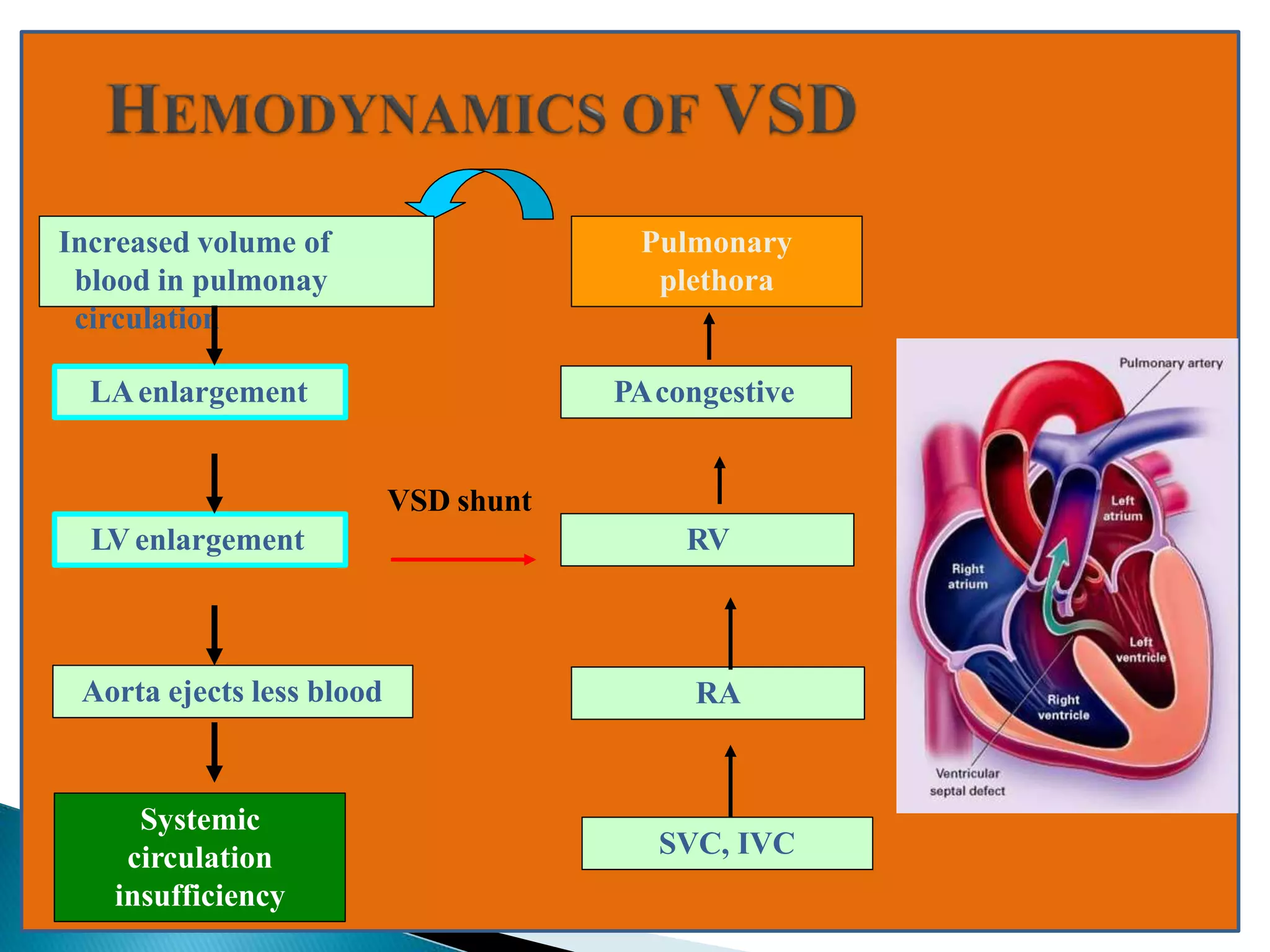
- VSDs can range in size from small and restrictive to large and non-restrictive, determining the amount of blood shunting between the ventricles and resulting hemodynamic consequences. Surgical closure is usually recommended for large non-restrictive defects to prevent long term pulmonary issues.