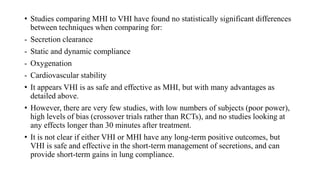
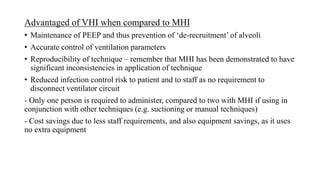
Ventilator hyperinflation (VHI) is a physiotherapy technique used in intubated patients on mechanical ventilation. It delivers larger tidal volumes than normal ventilation settings to improve lung function. The goals are to mobilize secretions, improve oxygenation, and re-expand atelectatic lung tissue. VHI has several advantages over manual hyperinflation, including maintaining PEEP levels, controlling ventilation parameters accurately, and reducing infection risks. Studies show VHI is as effective as manual methods in improving respiratory mechanics and gas exchange, while allowing reproducible administration of higher volumes safely.