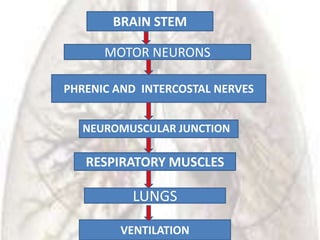
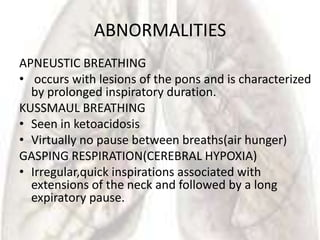
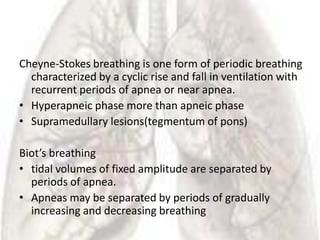
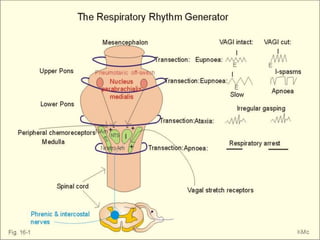
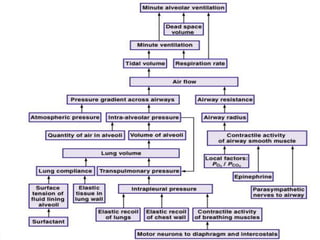
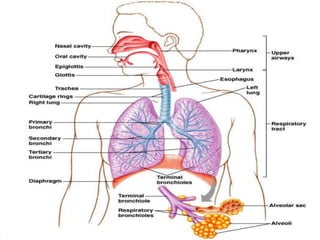
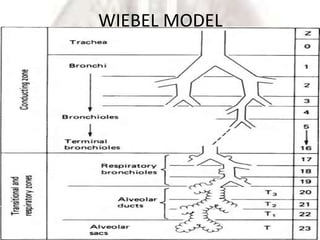
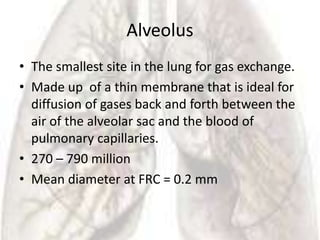
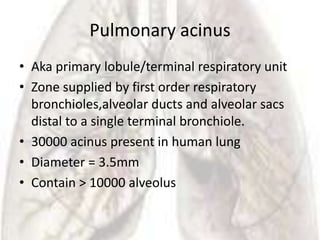
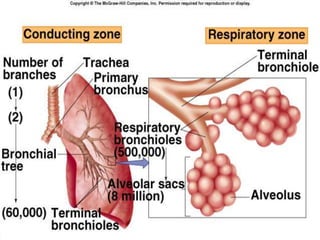
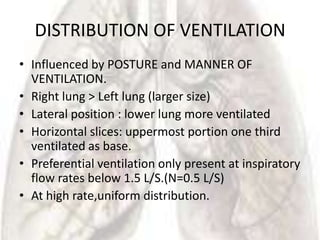
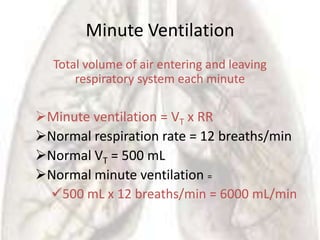
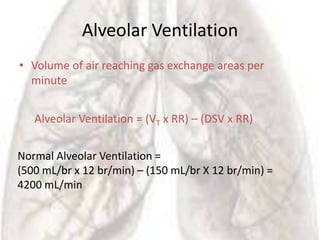
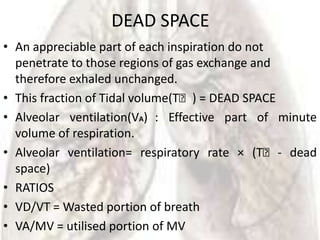
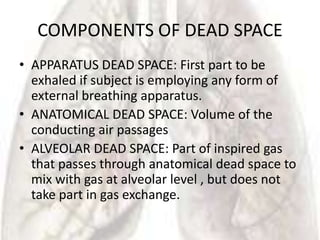
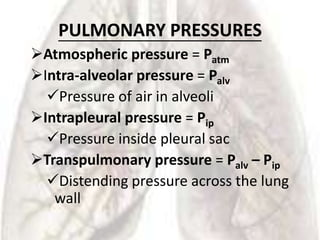
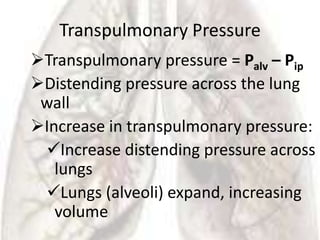
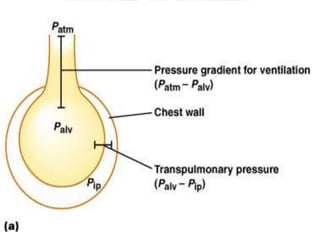
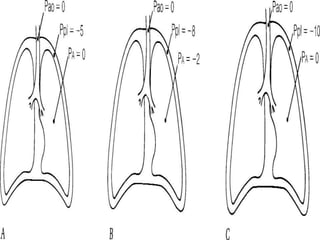
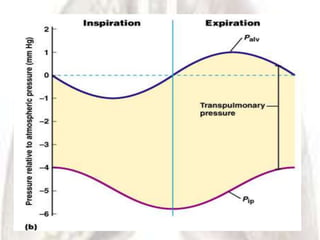
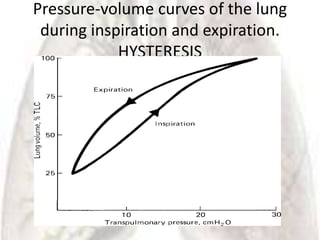
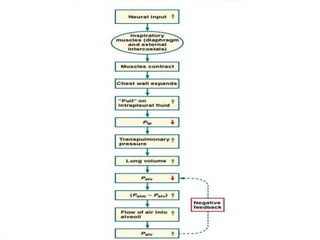
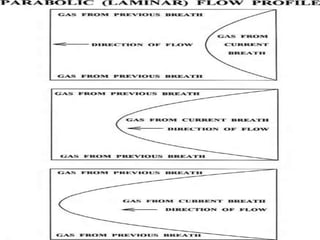
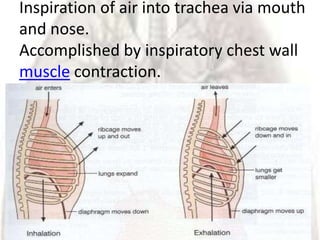
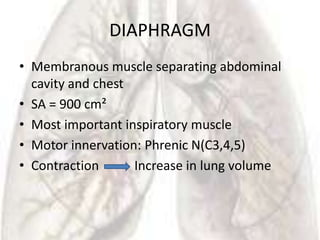
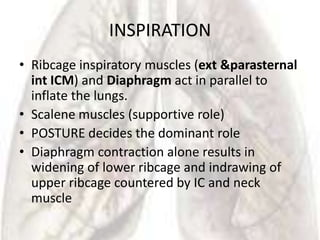
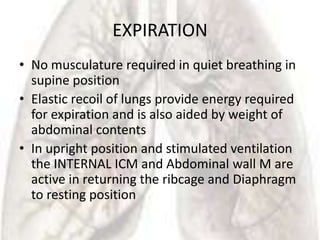
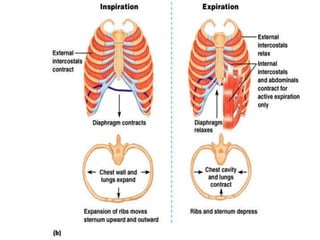
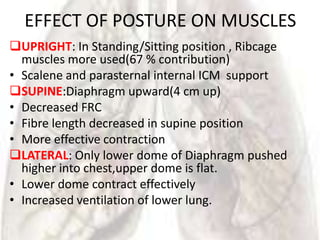
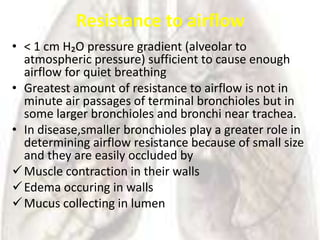
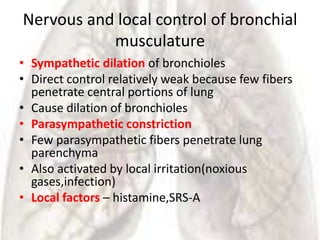
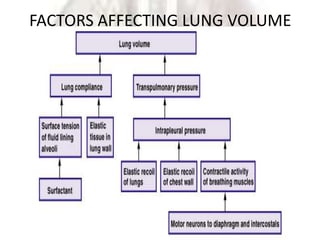
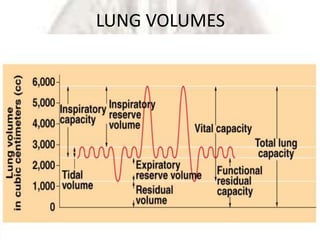
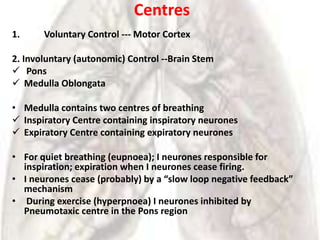
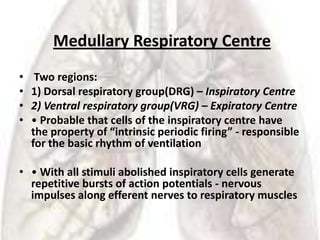
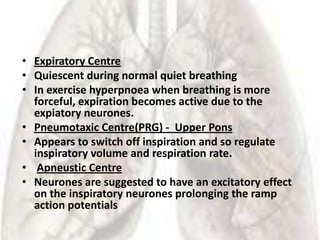
The document provides information on ventilation and the anatomy of the respiratory system. It defines ventilation as the mass movement of gas in and out of the lungs. It then describes the anatomy of the airways from the nostrils down to the alveoli. This includes details on structures like the nasal cavity, pharynx, larynx, trachea, bronchi, and terminal bronchioles. It also discusses factors that affect ventilation like pulmonary pressures, the mechanics of breathing, and control of breathing.

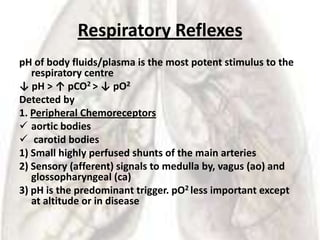
![Central Chemoreceptors
Surface of the Medulla Oblongata
• Measure pH of cerebrospinal fluid (CSF) and brain tissue
fluid
• Main aim of respiratory control is brain pH homeostasis
Hydrogen ions [H+] do not freely pass blood/CSF barrier
• But CO2 does easily (no lactic acid effect on central
chemoreceptors)
• In CSF CO2 + H2O = H+ + [HCO3 ] - H+ liberated then influences
the central chemoreceptors](https://image.slidesharecdn.com/ventilationfinal-120325205143-phpapp02/85/Ventilation-final-73-320.jpg)