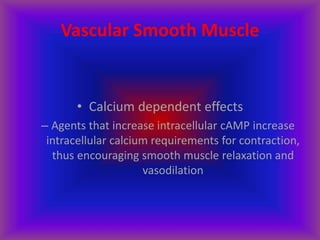
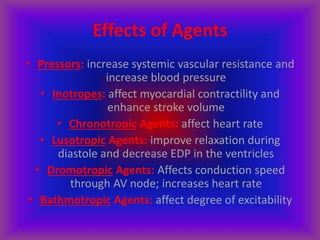
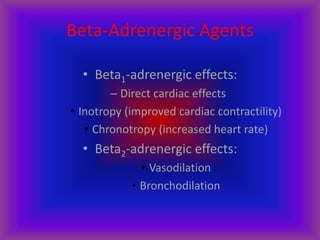
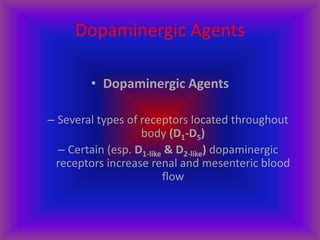
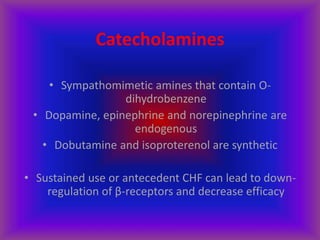
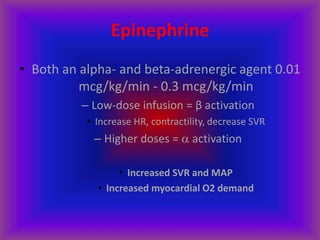
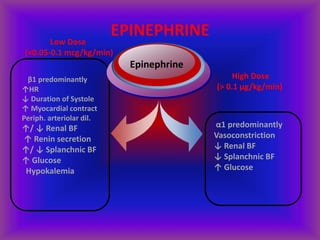
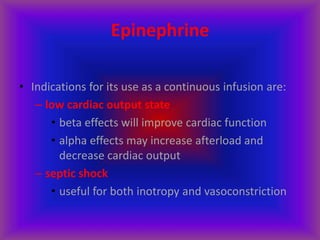
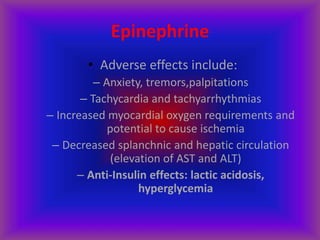
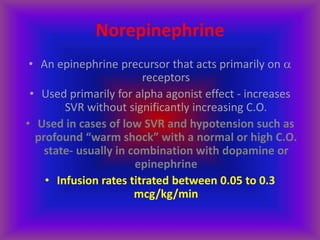
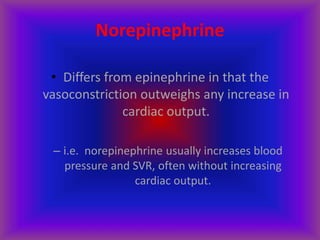
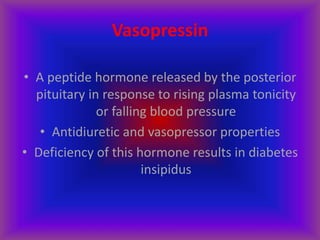
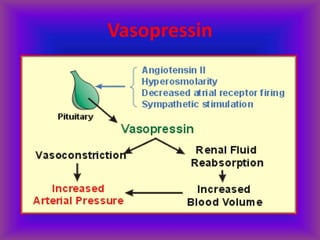
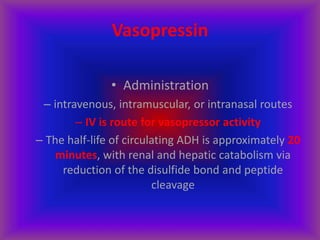
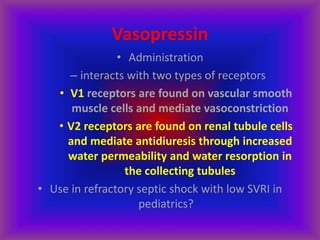
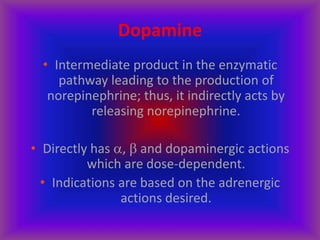
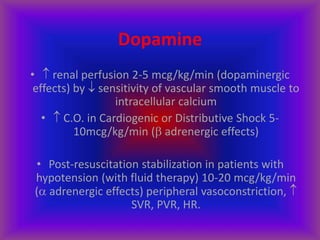
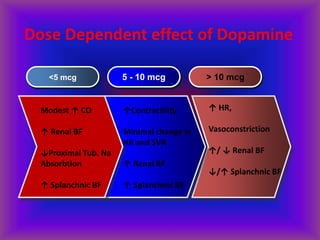
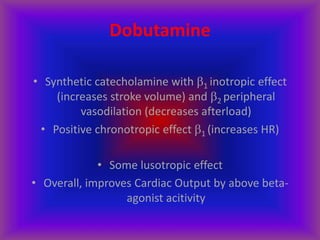
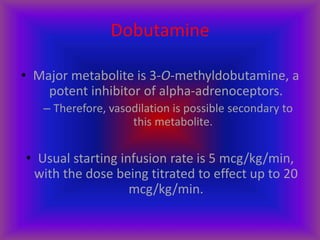
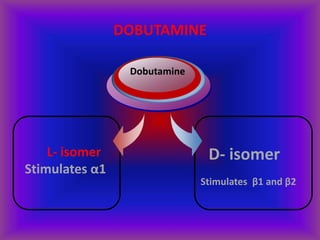
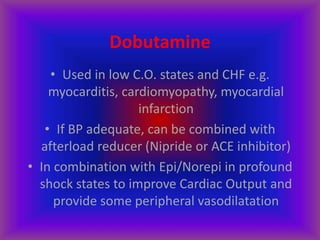
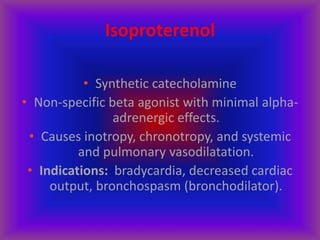
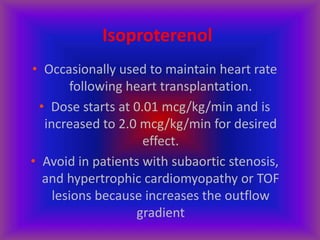
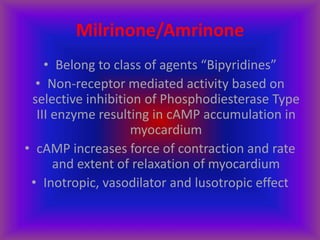
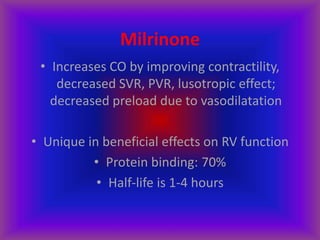
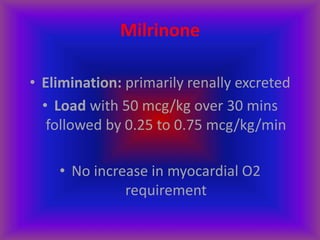
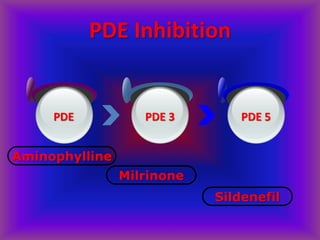
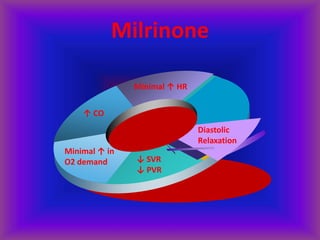
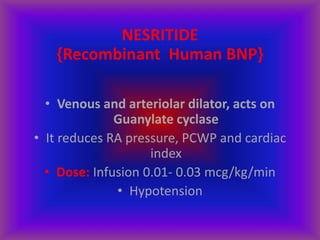
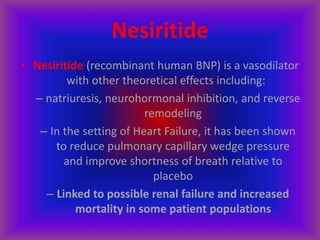
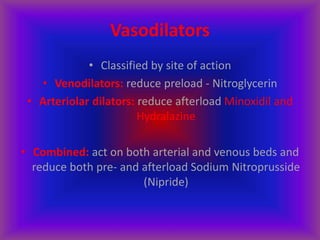
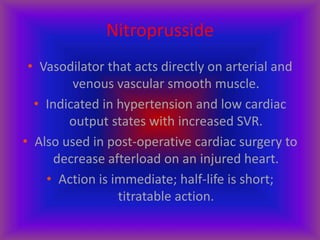
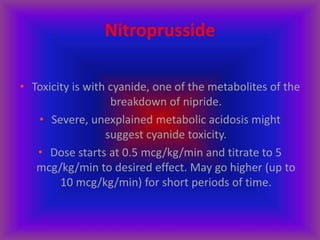
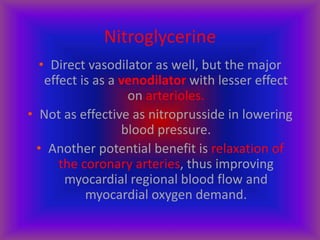
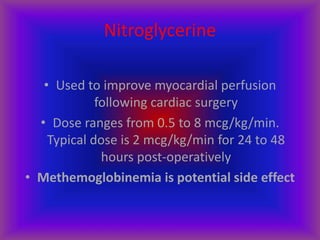
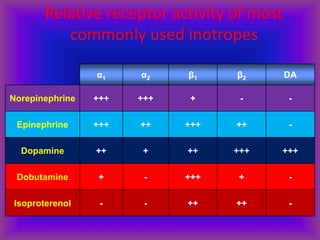
This document discusses various vasoactive drugs used to treat low blood pressure and cardiac issues in critically ill patients. It begins by explaining the immature heart's limited responsiveness to medications and calcium regulation. It then describes different types of effects that agents can have including increasing blood pressure, contractility, heart rate, and relaxation. The remainder of the document delves into specific drugs, outlining their mechanisms, indications, dosages, and side effects. These include catecholamines like epinephrine, norepinephrine, and dopamine, as well as dobutamine, milrinone, vasopressin, nitroprusside, and nesiritide.