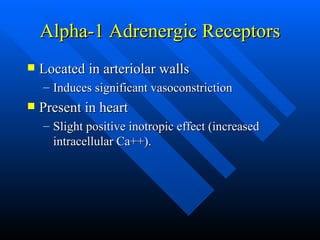
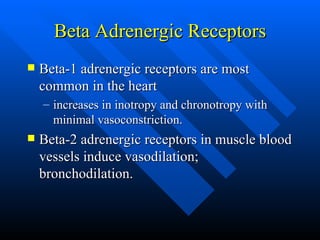
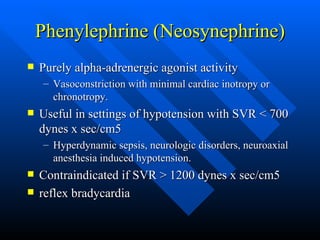
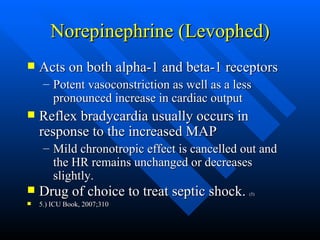
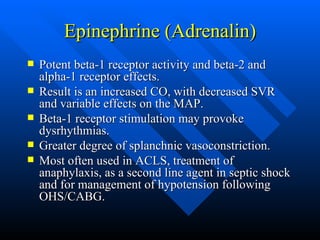
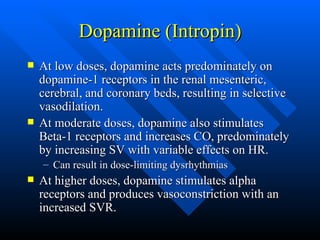
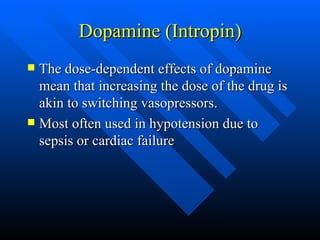
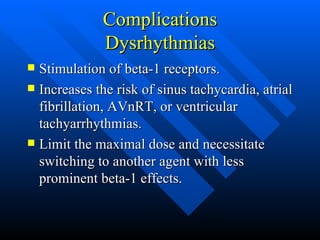
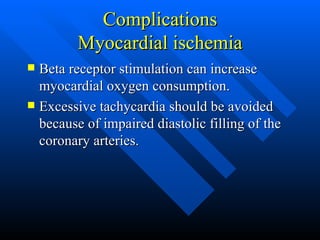
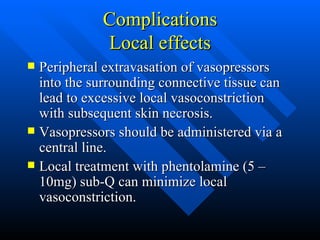
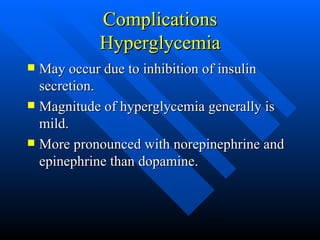
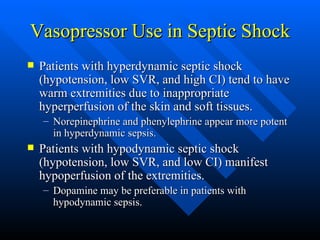
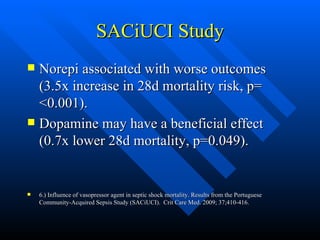
This document summarizes different vasopressors and inotropes used to treat hypotension. It describes the receptor activities, physiological effects, indications, and complications of various drugs including phenylephrine, norepinephrine, epinephrine, dopamine, dobutamine, vasopressin, and phosphodiesterase inhibitors. It provides guidance on selecting agents and titrating doses based on the underlying cause of hypotension and the patient's clinical status.