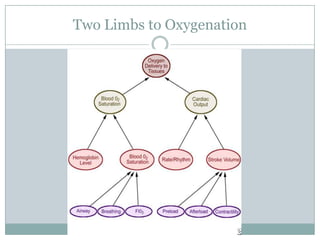
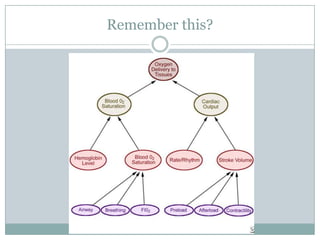
This document provides an overview of inotropes and vasoactive drugs, explaining how they work to increase cardiac output by enhancing contractility, heart rate, preload, and manipulating vascular resistance through their effects on adrenergic receptors and other mechanisms. It discusses various drugs like adrenaline, noradrenaline, dobutamine, vasopressin, GTN, and others, explaining their receptor targets, clinical applications, and nursing considerations for safe administration. The goal is to help nurses better understand these important hemodynamic medications and feel more confident in their use.