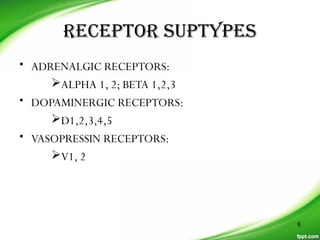
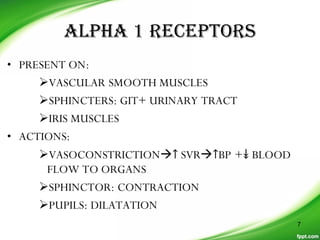
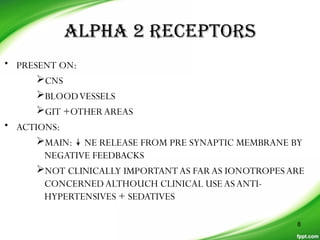
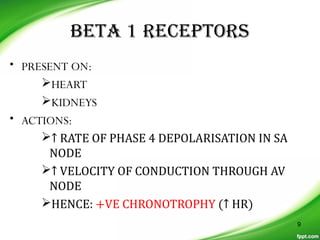
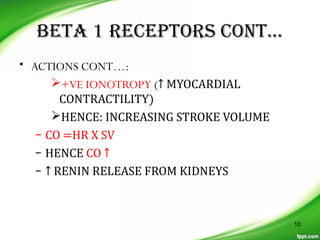
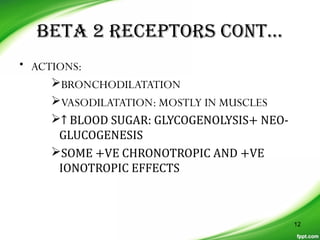
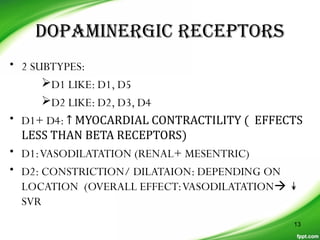
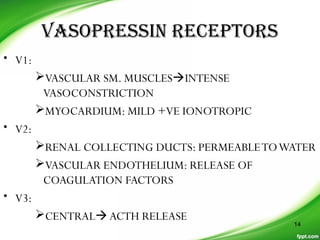
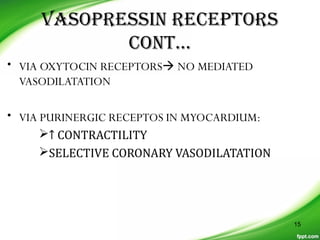
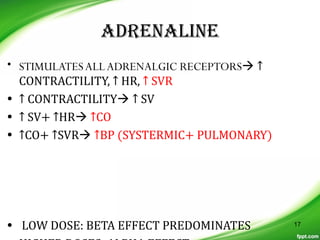
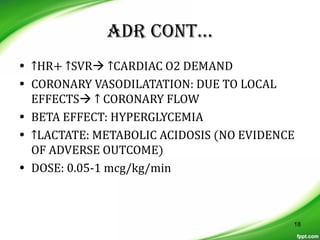
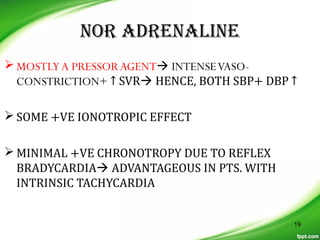
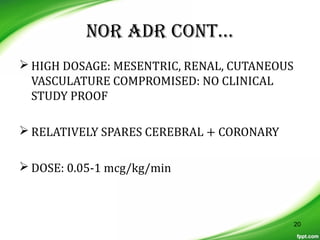
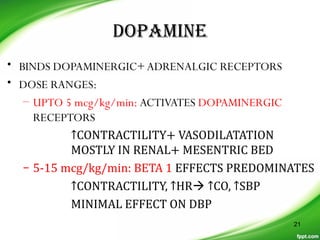
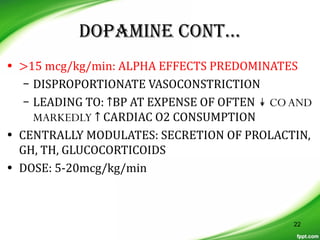
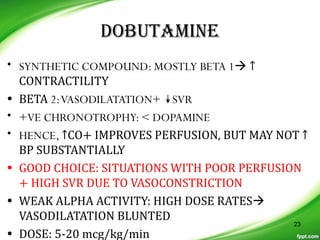
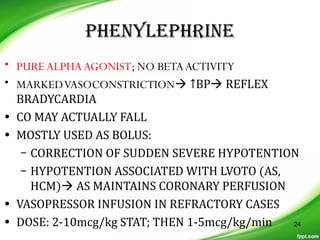
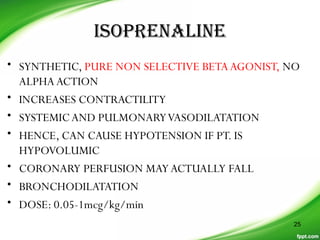
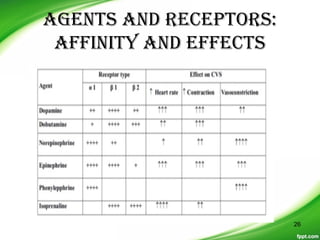
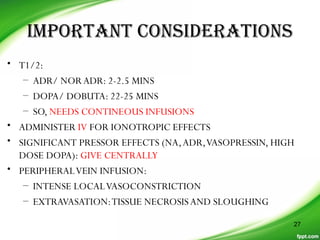
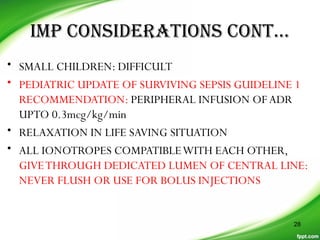
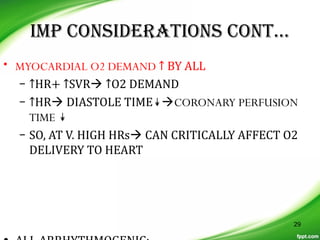
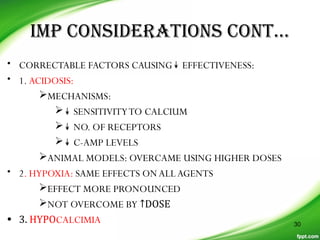
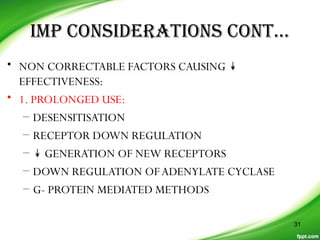
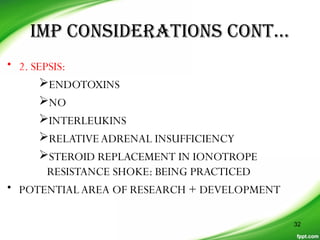
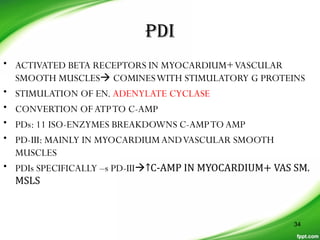
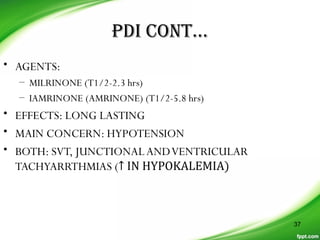
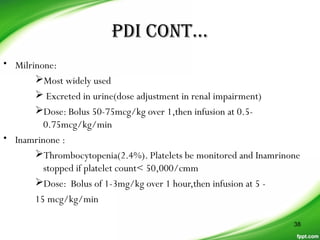
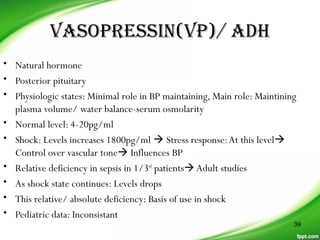
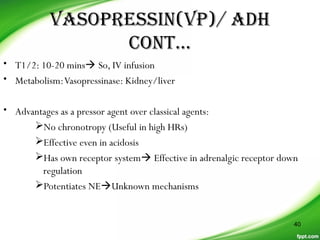
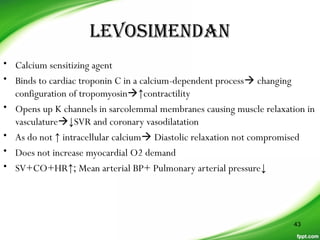
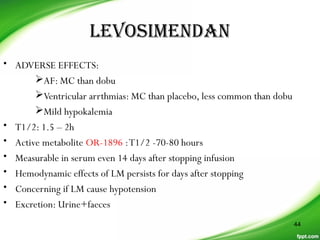
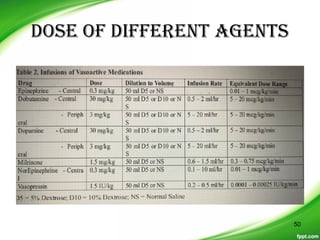
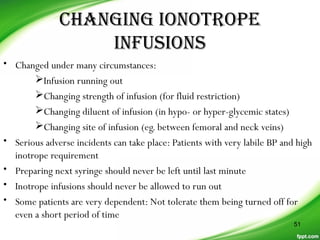
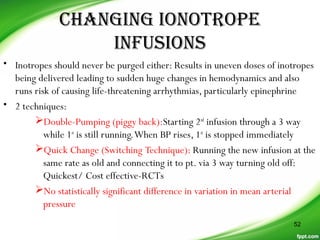
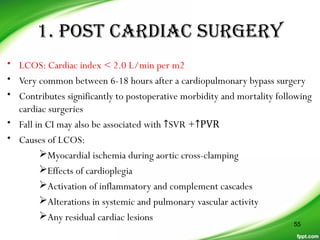
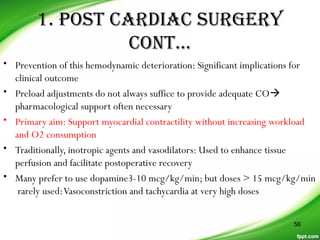
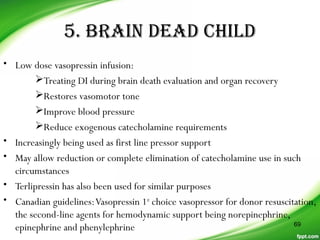
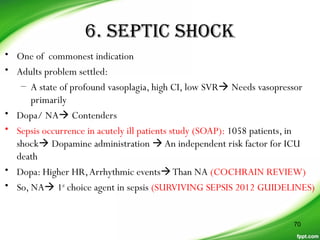
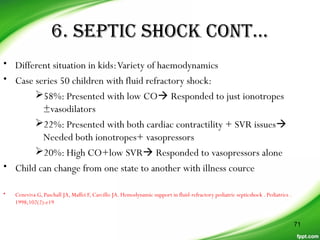
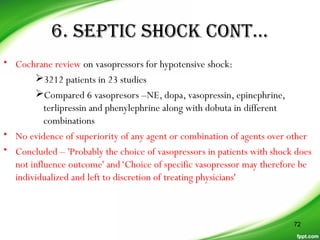
The document reviews the use of ionotropes in pediatric practice, describing the receptor subtypes targeted by various ionotropic drugs, the pharmacology and effects of individual agents like adrenaline, noradrenaline, dopamine, and dobutamine, important considerations for drug administration, and newer agents like phosphodiesterase inhibitors and vasopressin.