1) Beta blockers may help reduce mortality and improve outcomes in patients with traumatic brain injury by attenuating the hyperadrenergic response and decreasing cardiac complications.
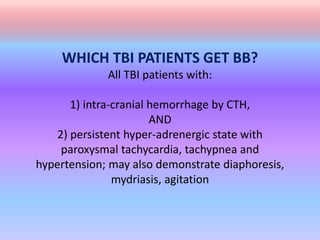
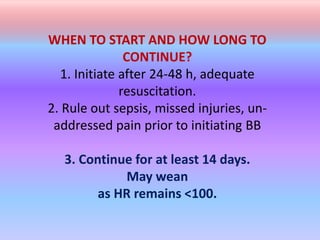
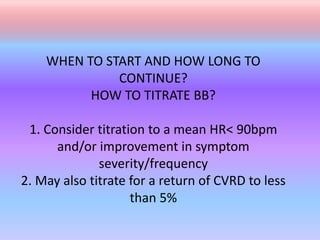
2) Patients with TBI who have intracranial hemorrhage and a persistent hyperadrenergic state may benefit from beta blockers like propranolol or labetalol to control tachycardia, hypertension, and other symptoms.
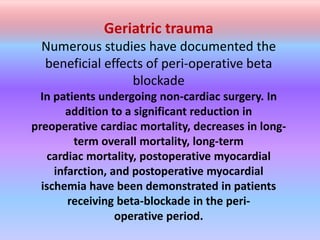
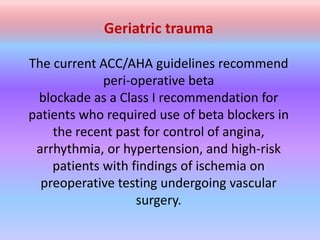
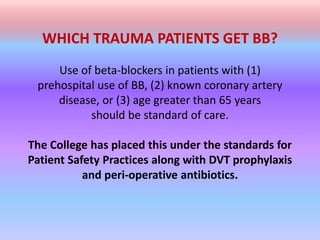
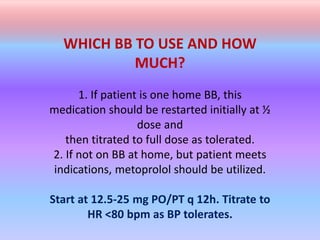
3) Beta blockers may also improve outcomes for geriatric trauma patients and those with pre-existing cardiac conditions by reducing postoperative cardiac risks when started pre-operatively and continued peri-operatively.