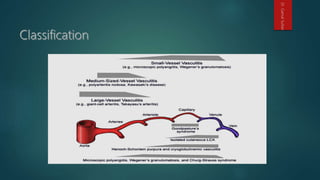
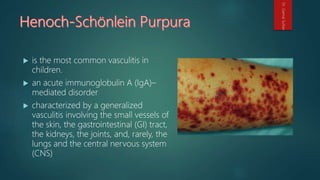
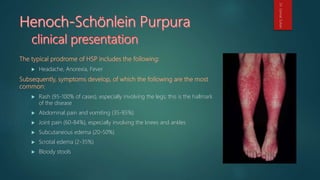
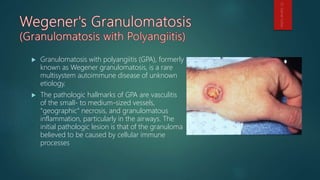
Vasculitis refers to inflammation of blood vessels. It can present with a variety of clinical manifestations depending on the size of vessels involved. The Chapel Hill Consensus Conference created a classification system for major types of vasculitis including Wegener's granulomatosis, Churg-Strauss syndrome, and microscopic polyangiitis. Henoch-Schönlein purpura is the most common vasculitis in children, characterized by a vasculitis involving small vessels of the skin, GI tract, kidneys, joints, and rarely lungs and CNS, with IgA deposits in vessel walls. Granulomatosis with polyangiitis is a multisystem disease involving vasculitis of small to medium


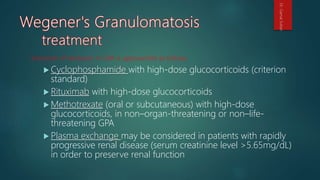
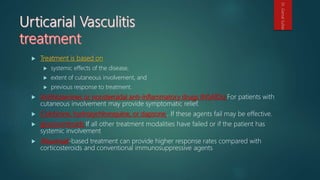
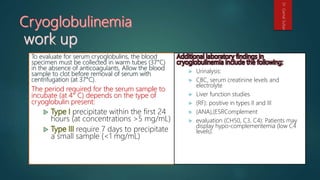
![Maintenance of remission
Once induction of remission has occurred, treatment for
maintenance of remission should be continued for at least 18
months, often longer
Azathioprine (2 mg/kg/day) is safer than, and as effective as,
cyclophosphamide in maintaining remission [6]
Methotrexate (20-25 mg weekly, oral or subcutaneous) has been
used for the maintenance of remission if the serum creatinine level
is less than 1.5 mg/dL
Leflunomide (20-30 mg/day) is as effective as methotrexate, but it
is associated with more adverse effects
Dr.GamalSultan](https://image.slidesharecdn.com/vasculites-160906203924/85/Vasculitis-33-320.jpg)
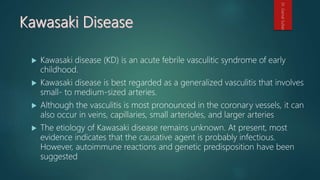
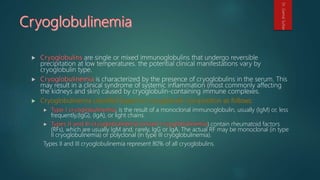
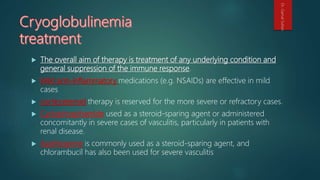
![ No specific laboratory test is used to diagnose Kawasaki disease (i.e., [ESR], [CRP]
and alpha1-antitrypsin levels) are elevated at first; then return to baseline 6-10
weeks after the onset of the illness.
More recently, 2 urine proteins hold as biomarkers of Kawasaki disease: meprin A
or filamin C.
Elevated macrophage migration factor (MIF) and (IL-6) may be useful markers in
the acute stages of Kawasaki disease.
(CBCs) normochromic anemia, (WBC) is moderate to high (50% of patients have a
WBC greater than 15,000/µL), with a left shift
Thrombocytopenia is associated with severe coronary artery disease and
myocardial infarction. rarely, it may be associated with disseminated intravascular
coagulation.
Serum cholesterol, high-density lipoprotein, and apolipoprotein A levels are
decreased;
Dr.GamalSultan](https://image.slidesharecdn.com/vasculites-160906203924/85/Vasculitis-50-320.jpg)
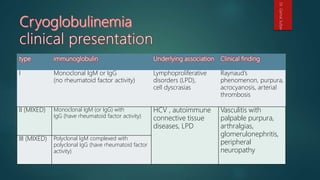
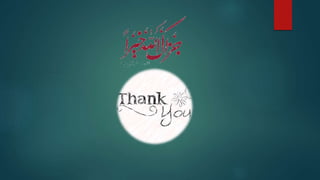
![The principal goal of treatment is to prevent coronary artery disease and to relieve symptoms.
Full doses of intravenous immunoglobulin (IVIG) are the mainstay of treatment.
Aspirin (high-dose, followed by low-dose) has traditionally been standard.
Other medications include the following:
Corticosteroids: Typically in patients unresponsive to standard therapies
Methotrexate or cyclophosphamide: In IVIG-resistant cases
Infliximab: In refractory cases with coronary aneurysms [10]
Antiplatelet medications (eg, clopidogrel, dipyridamole
Anticoagulants (eg, warfarin, low-molecular-weight heparin
A new treatment ulinastatin (UTI), a neutrophil elastase inhibitor used to treat patients with
circulatory shock or pancreatitis.
Dr.GamalSultan](https://image.slidesharecdn.com/vasculites-160906203924/85/Vasculitis-51-320.jpg)
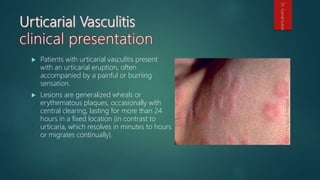
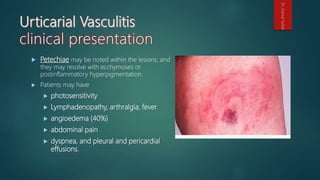
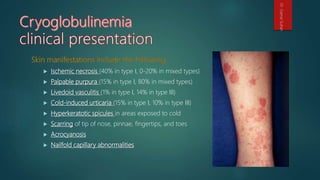
![ an eruption of erythematous wheals that clinically resemble urticaria but
histologically show changes of leukocytoclastic vasculitis.
Urticarial vasculitis may be divided into normocomplementemic and
hypocomplementemic variants.
Both subsets can be associated with systemic symptoms (eg,angioedema,
arthralgias, abdominal or chest pain, fever, pulmonary disease, renal disease,
episcleritis, uveitis, and Raynaud phenomenon).
The hypocomplementemic form more often is associated with systemic symptoms
and has been linked to connective-tissue disease (ie, [SLE]).
Dr.GamalSultan](https://image.slidesharecdn.com/vasculites-160906203924/85/Vasculitis-64-320.jpg)