The document provides a comprehensive overview of systemic vasculitis, including its clinical features, classification, diagnostic criteria, and management strategies. It discusses specific types of vasculitis such as giant cell arteritis, granulomatous polyangiitis, and microscopic polyangiitis, and emphasizes the importance of identifying symptoms and conducting appropriate tests for accurate diagnosis. Additionally, it highlights the complicated nature of vasculitis and the necessity for careful patient assessment and differential diagnosis.














![COMPLEX MEDICAL PROBLEMS 2
Develop a strategy: PROBLEM LIST
CREATE PROBLEM LIST
……… LIST EVERYTHING [split don’t lump]
PRIORITIZE PROBLEM LIST
……… WHAT’S THE BIG GORILLA(S) HERE?
“WORK” the PROBLEM LIST](https://image.slidesharecdn.com/2015systemicvasculitis-240611043634-ac662bc8/75/2015-mangement-of-Systemic-Vasculitis-ppt-16-2048.jpg)















































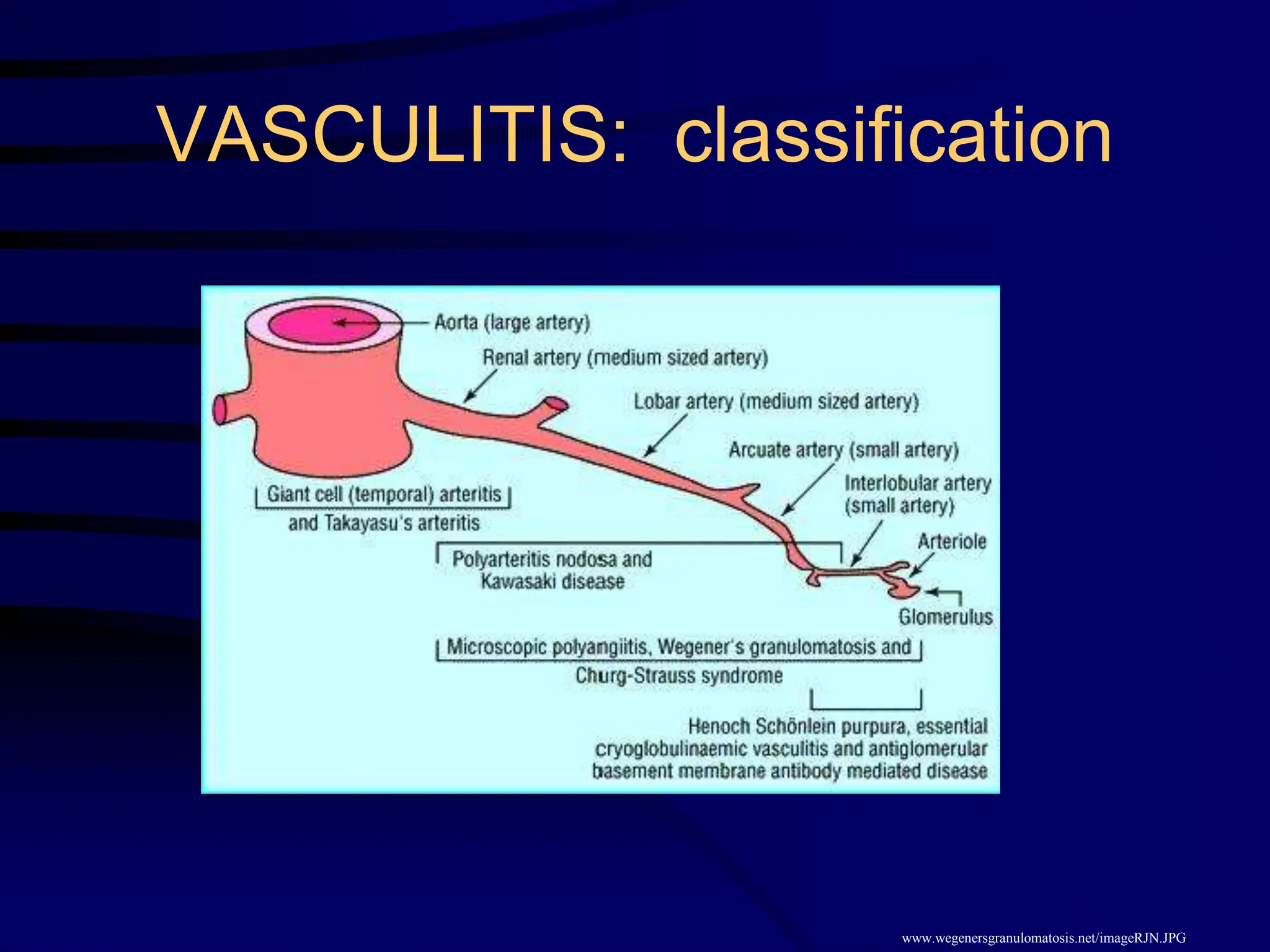
![VASCULITIS OF SMALL >> MEDIUM-SIZED
VESSELS:
• drug-induced small vessel vasculitis
(hypersensitivity vasculitis),
• Henoch-Schönlein purpura (IgA vasculitis),
• ANCA-associated vasculitis
(granulomatosis with polyangiitis [Wegener’s],
microscopic polyangiitis, eosinophilic granulomatosis
with polyangiitis [Churg Strauss syndrome]),
• infection-related vasculitis
(bacterial endocarditis, poststreptococcal vasculitis
and glomerulonephritis) plus hepatitis C-related
cryoglobulinemia)](https://image.slidesharecdn.com/2015systemicvasculitis-240611043634-ac662bc8/75/2015-mangement-of-Systemic-Vasculitis-ppt-64-2048.jpg)
