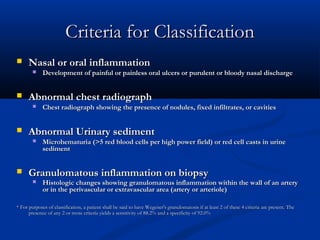
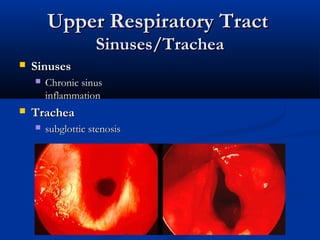
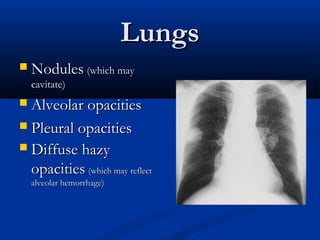
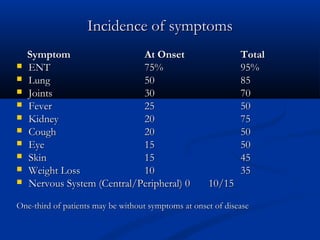
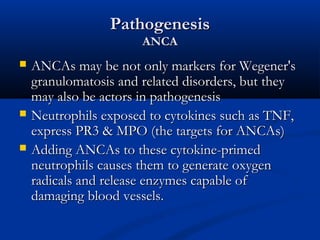
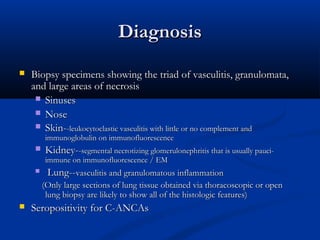
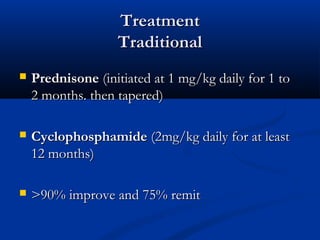
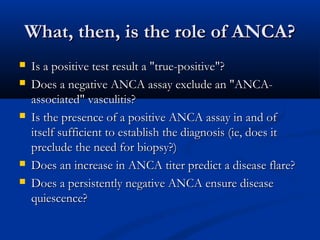
Wegener's granulomatosis is a necrotizing vasculitis characterized by inflammation of blood vessels. It commonly involves the respiratory tract and kidneys. Diagnosis is based on clinical criteria including nasal or oral inflammation, lung abnormalities on chest imaging, hematuria or red blood cell casts on urinary sediment, and granulomatous inflammation on biopsy. The disease is associated with positive testing for PR3-ANCA. Treatment involves corticosteroids and cyclophosphamide or methotrexate to induce remission, though relapses are common due to toxicity of cyclophosphamide. The role of ANCA testing in diagnosis and monitoring disease activity requires further clarification.