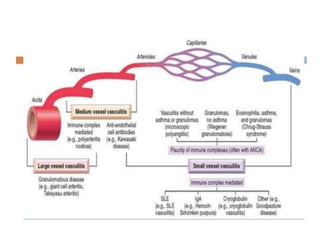
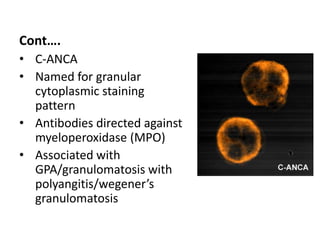
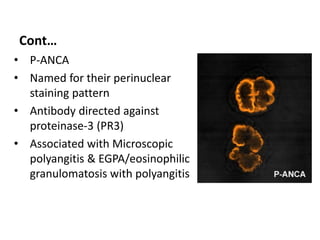
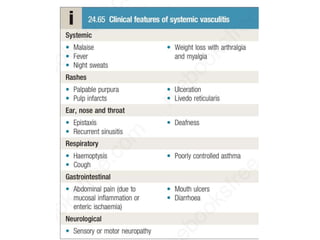
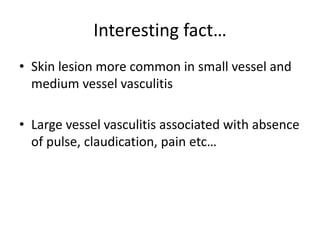
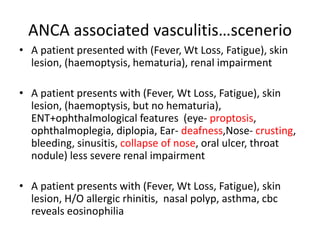
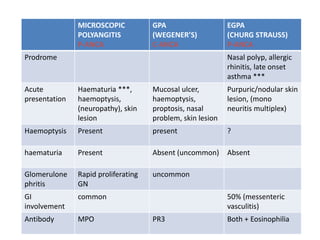
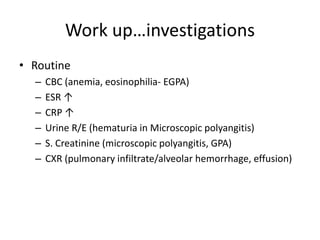
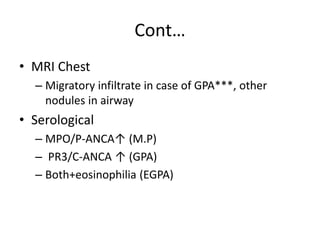
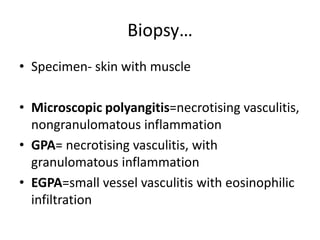
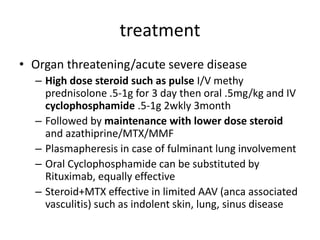
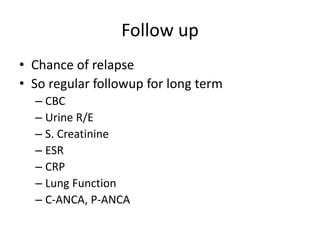
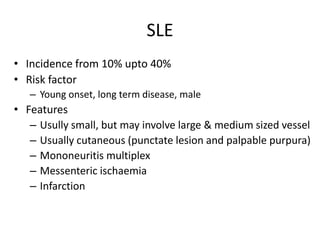
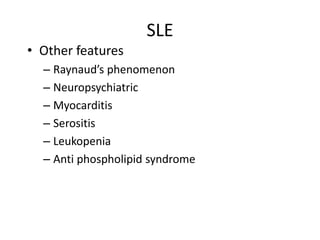
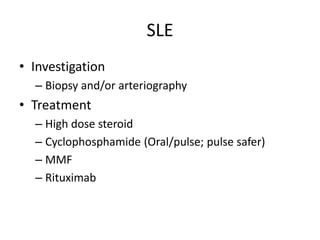
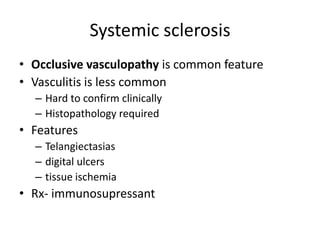
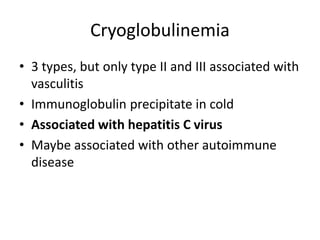
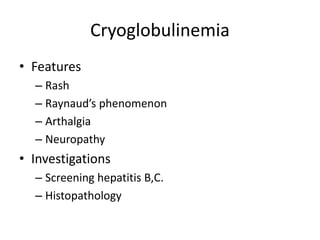
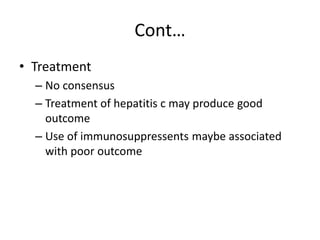
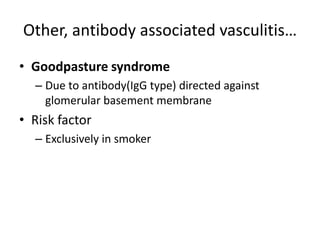
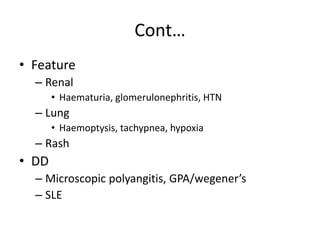
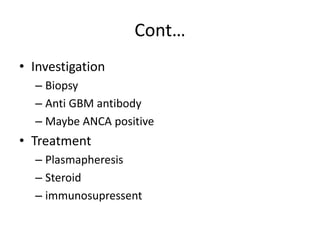
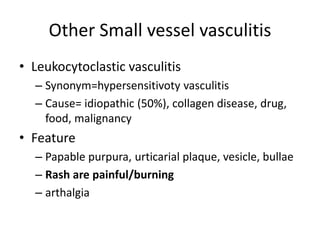
This document summarizes different types of small vessel vasculitis. It defines vasculitis as inflammation and damage of blood vessel walls. It describes common clinical features and divides vasculitis by vessel size involved - large, medium, small. It provides detailed information on ANCA-associated vasculitis including definitions, types of ANCA, associated diseases, investigations and treatment. Other small vessel vasculitis discussed include immune complex mediated types like SLE and cryoglobulinemia.