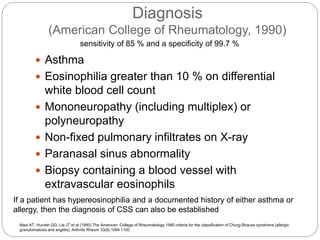
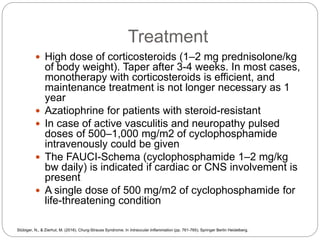
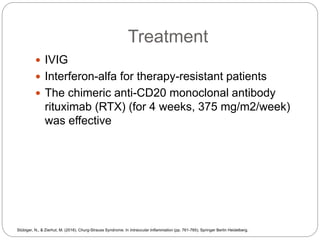
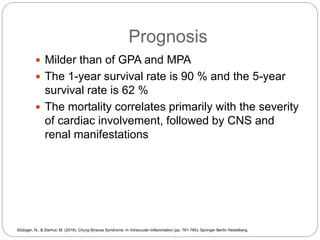
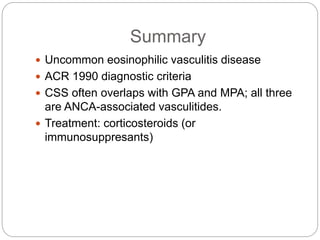
This document defines and outlines Churg-Strauss Syndrome (CSS), a rare eosinophilic vasculitis disease. It provides details on the epidemiology, pathogenesis, clinical manifestations, diagnosis, treatment, and prognosis of CSS. CSS is characterized by eosinophil-rich inflammation involving small to medium blood vessels and is associated with asthma, allergies, and eosinophilia. Treatment involves high doses of corticosteroids, with immunosuppressants used for resistant cases. Prognosis is generally better than other vasculitis diseases but mortality can occur from cardiac or neurological involvement.