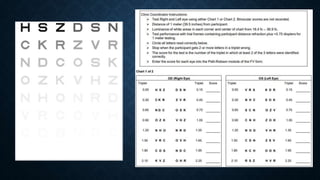
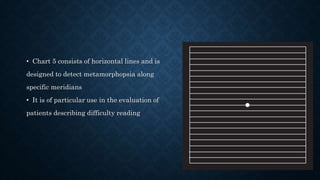
Visual acuity and contrast sensitivity are measures of visual function. Visual acuity is a measure of visual resolution and is affected by optical and physiological factors. It can be measured using letters of decreasing size on charts like the Snellen chart. Contrast sensitivity measures the ability to detect differences in luminance and is more relevant to daily vision tasks. It is assessed using gratings of varying contrast and spatial frequency. The Amsler grid is used to screen for macular diseases by having patients look for visual distortions or gaps within a grid viewed at the fovea.