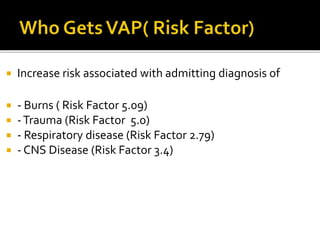
The document outlines the risks and prevention strategies associated with ventilator-associated pneumonia (VAP) in intubated patients. It details factors that increase the risk, the importance of oral hygiene, head positioning, and sedation management in preventing VAP. It also emphasizes the need for adequate staffing and effective oral care protocols to reduce the incidence of hospital-acquired pneumonia in mechanically ventilated patients.








![ A. First:- First, encourage and advocate for the use of non-
invasive ventilation approaches, such as bi-level positive airway
pressure or continuous positive airway pressure.
B. Second:- Second, when mechanical ventilation can’t be
avoided, work to minimize its duration. Ventilator-weaning
protocols or evidence-based care bundles (for example, the
Awakening, Breathing Coordination, Delirium, and Early mobility
[ABCDE] bundle) can be effective in shortening mechanical
ventilation duration.](https://image.slidesharecdn.com/vap-200413121032/85/VAP-14-320.jpg)









