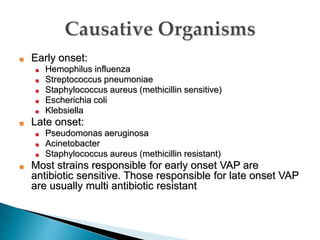
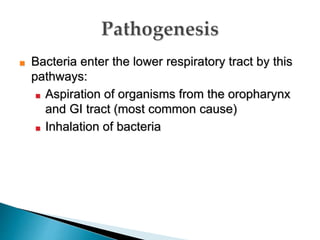
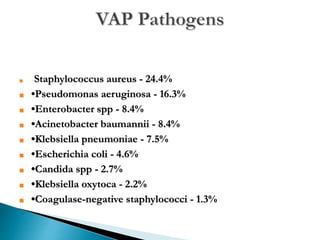
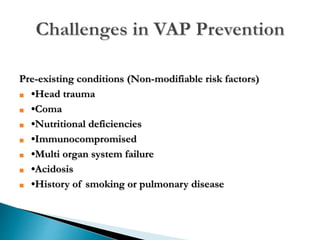
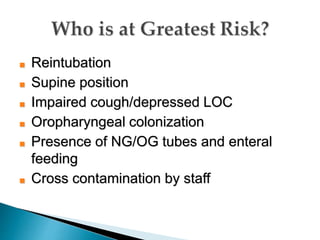
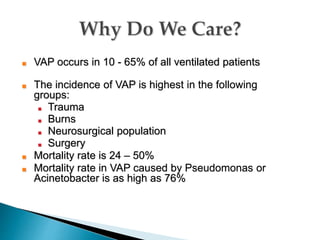
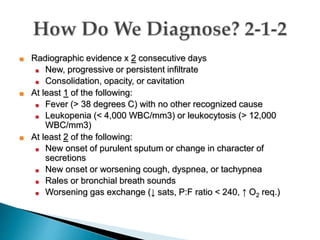
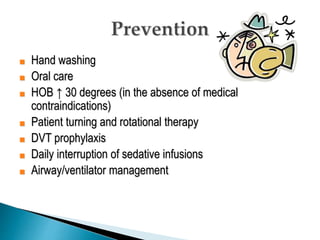
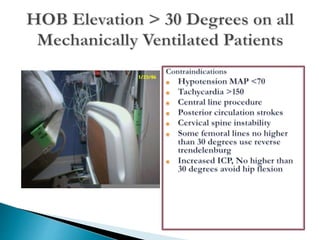
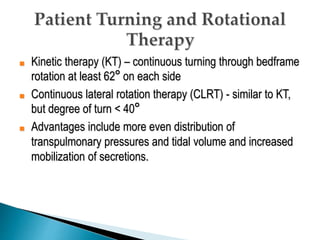
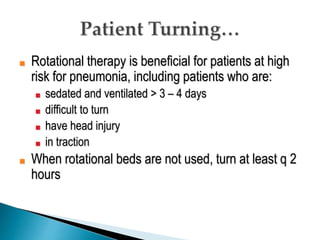
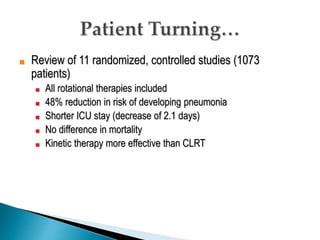
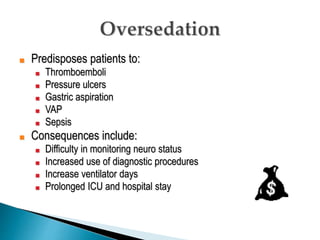
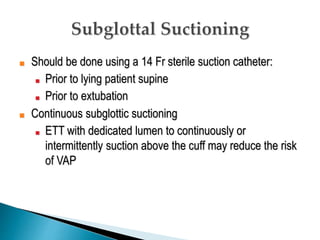
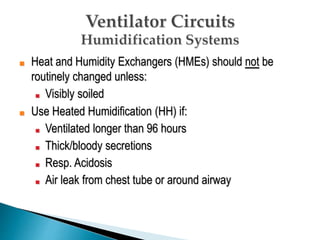
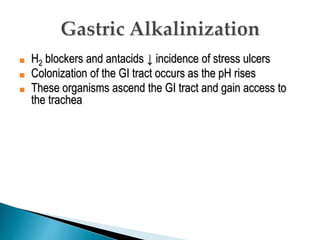
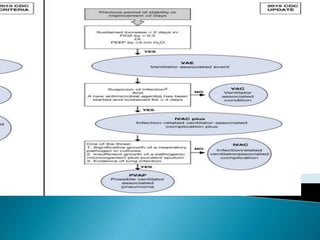
This document defines ventilator-associated pneumonia (VAP) and identifies factors that increase risk. It also outlines effective strategies for reducing VAP incidence, including proper hand hygiene, oral care, keeping patients' heads of bed elevated, rotational therapy for immobile patients, limiting sedation, and following best practices for ventilation and airway management. Regular monitoring and a multidisciplinary team approach can help implement evidence-based guidelines to decrease VAP rates.