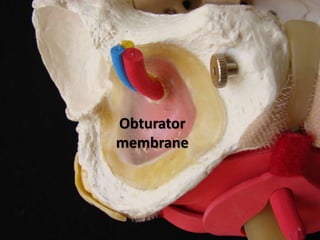
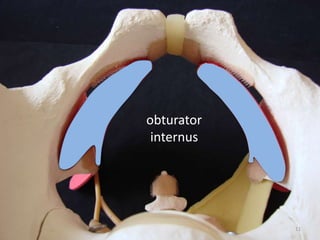
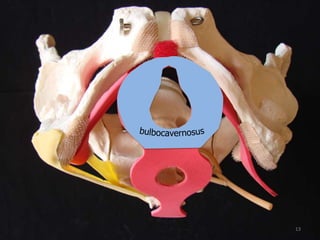
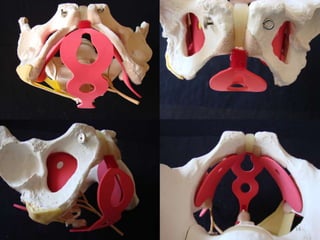
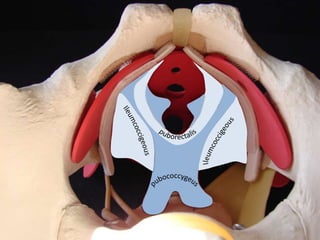
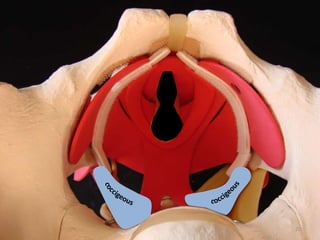
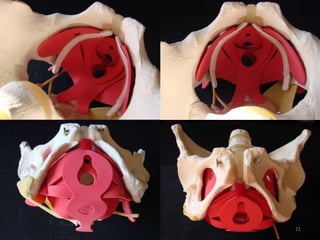
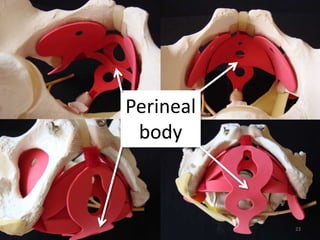
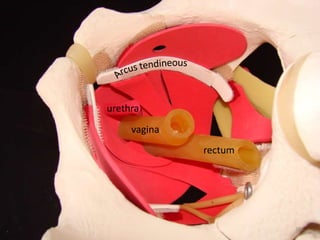
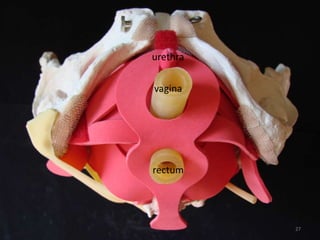
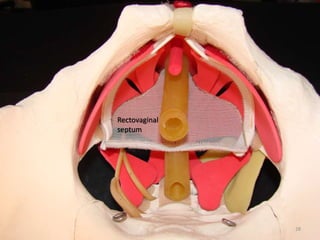
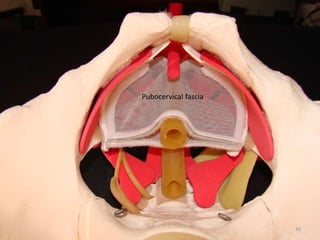
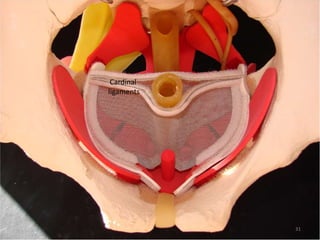
This document provides an overview of the 3-D surgical anatomy of the female pelvis. It lists the coordinators and faculty of the course and then covers the bones, ligaments, muscles, viscera and fascias of the female pelvic region. Images are included to illustrate key anatomical structures like the pubic bone, obturator foramen, levator ani muscles, vagina, rectum, urethra and fascial planes in the pelvis.