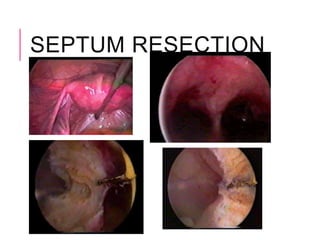
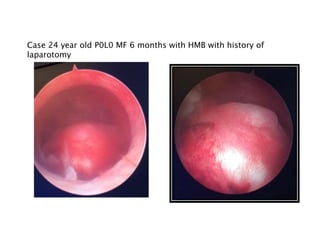
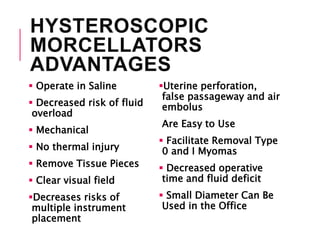
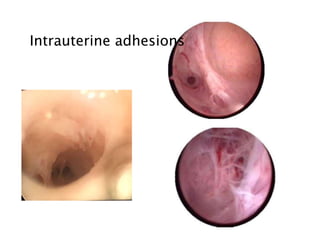
This document provides information on operative hysteroscopy, including prerequisites, contraindications, instrumentation, anaesthesia, distension media, indications, and techniques for various procedures like endometrial ablation, uterine septum resection, myomectomy, and adhesiolysis. It discusses the advantages and disadvantages of hysteroscopic morcellators. Complications of hysteroscopic myomectomy and post-operative care are also outlined. Various classifications for submucous fibroids and intrauterine adhesions are presented.