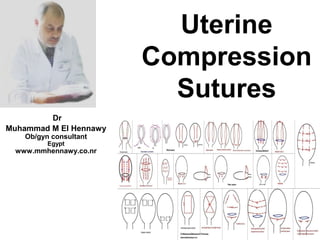
This document discusses uterine compression sutures as a technique to control postpartum hemorrhage. It begins by explaining that postpartum hemorrhage is the leading cause of maternal mortality worldwide. Uterine compression sutures involve applying sutures externally to the uterus in various patterns to promote uterine contraction and compression of blood vessels, similar to manual compression. The sutures act as a brace for the uterus. Indications for uterine compression sutures include atonic PPH, abnormal placentation, coagulopathy, and as prophylaxis for high risk patients. Both absorbable and non-absorbable suture materials can be used.